More pain education urgently needed, leading specialist says
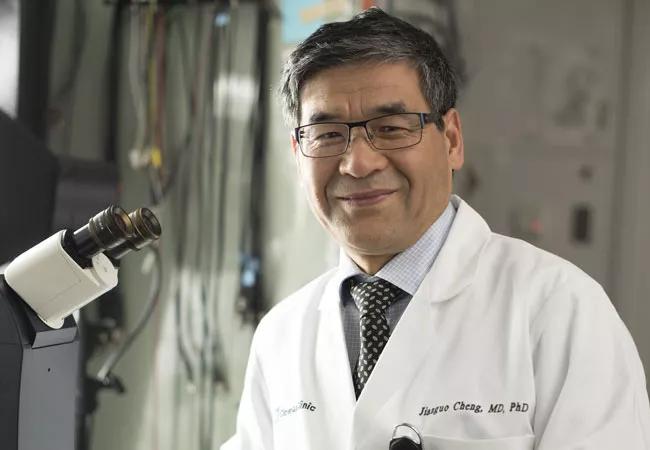
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/41133040-34fd-4cd3-b888-2dd5f079329b/19-PAI-1431_Cheng_CQD_650x450_1-002_jpg)
19-PAI-1431_Cheng_CQD_650x450_1 (002)
Pain is a hugely important but woefully misunderstood aspect of medicine that has taken on even more urgency in the throes of the opioid crisis, which claims 130 lives daily. More than 50 million Americans suffer from chronic pain, making it the number-one reason people go to a physician. That conservative estimate doesn’t include members of the military, the prison population or patients under the age of 18.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
And yet, most medical schools and residencies teach almost nothing about pain diagnosis and treatment, those that do don’t teach nearly enough, and U.S. licensing exams do little to test clinicians’ understanding of pain mechanisms and management strategies, says Jianguo Cheng, MD, PhD, Director of the Multidisciplinary Pain Management Fellowship at Cleveland Clinic.
Dr. Cheng, his colleagues at Cleveland Clinic and his co-members on two national committees, are on a mission to change that.
“Most physicians are trained to believe pain is a symptom of other diseases and that if they treat the disease, the pain will go away. This is not the case,” says Dr. Cheng, who is also immediate past president of the American Academy of Pain Medicine (AAPM).
To tackle these shortcomings, under Dr. Cheng’s leadership, AAPM has named pain education a strategic priority and is working on a wide-ranging plan to define core competencies for clinicians; develop educational content; overcome barriers to patient and public awareness; and identify which approaches work best.
Representing AAPM and Cleveland Clinic, Dr. Cheng serves on the Health Professional Education and Training Working Group of the National Academy of Medicine Action Collaborative on Countering the U.S. Opioid Epidemic and on the Department of Health and Human Services Pain Management Best Practices Inter-Agency Task Force. The Task Force submitted a Final Report to Congress in May updating best practices and providing recommendations to address pain treatment gaps and inconsistencies.
Advertisement
Education, credentialing and licensing focused on safe and effective pain assessment and management would improve pain treatment and mitigate factors contributing to the opioid crisis, according to the report, which notes that fewer than 20% of the more than one million health providers licensed to prescribe controlled substances have training on how to prescribe opioids safety and effectively.
Despite recent decreases in the number of opioids prescribed, many physicians continue to rely too heavily on opioids to treat pain, says Dr. Cheng. Why? Because they didn’t learn in medical school or residency training about the various causes of pain or how to assess when a patient might benefit from an earlier referral for specialized care.
As a result, treatment often starts appropriately enough with the use of anti-inflammatory medication but quickly progresses to a low-dose opioid, followed by a stronger opioid if the patient doesn’t improve. Before long, many patients find themselves taking multiple strong opioids and heading down a dangerous path.
Complicating the picture is the fact that patients who suffer from anxiety and chronic pain may be prescribed a benzodiazepine, which can be fatal in combination with an opioid. In 2016, the FDA issued label requirements for prescription opioids and benzodiazepines to include a black box warning cautioning physicians of the risk of death in patients who take the drugs together.
Many of these scenarios could be prevented if clinicians learned about the variety of available non-opioid and opioid-sparing alternatives, including restorative and integrative approaches; physical and cognitive therapy; and interventional and surgical techniques, including radiofrequency ablation and nerve blocks.
Advertisement
Cleveland Clinic has established an Enterprise Pain Management Committee to reduce unnecessary exposure of patients to opioids systemwide. The Committee makes recommendations to clinicians and departments on how to more effectively manage acute and chronic pain that includes training in early, appropriate referral to pain management specialists, how to manage pain perioperatively, and how to identify patients with opioid use disorder so they can be referred to an addiction specialist. In addition, the Cleveland Clinic Annual Pain Management Symposium attracts more than 300 clinicians each year.
Dr. Cheng points to signs of progress. The recognition of pain as a category or subcategory of disease in the International Classification of Diseases, 11th Revision (ICD-11), recently released by the World Health Organization, heralds a step forward. For example, ICD-11 recognizes neuropathic pain as a category of neurological disease. Similarly, headaches, including migraines, are also recognized as a category of neurological disease. Most pain conditions, whether classified as a medical condition or a disease, now have a specific code for the first time.
Still, “many clinicians have a limited understanding of the complexities of pain diagnosis and treatment,” Dr. Cheng says. A long-term focus on pain education is urgently needed to keep the problem from escalating as the U.S. population rapidly ages.
Advertisement
Advertisement
Researchers seek solutions to siloed care, missed diagnoses and limited access to trauma-informed therapies
Study participants also reported better sleep quality and reduced use of pain medications
Two-hour training helps patients expand skills that return a sense of control
Program enhances cooperation between traditional and non-pharmacologic care
National Institutes of Health grant supports Cleveland Clinic study of first mechanism-guided therapy for CRPS
Pain specialists can play a role in identifying surgical candidates
Individual needs should be matched to technological features
New technologies and tools offer hope for fuller understanding