Pain specialists can play a role in identifying surgical candidates
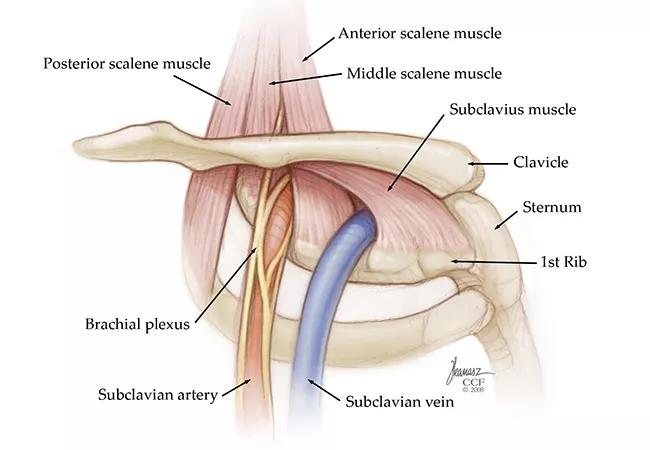
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/cfef58de-ac35-4362-84b1-914d3e745a45/22-PAI-3027274-CQD-650x450-1_jpg)
thoracic outlet syndrome illustration
A nurse developed neck pain and numbness that radiated down her right arm and into her clavicle and chest. She had severe symptoms while working with her hands over her head. The condition began without any particular inciting event, and only position change would relieve the symptoms, which greatly interfered with performing work duties.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Fearing a serious condition, she initially presented to her local hospital emergency department. She was referred to Cleveland Clinic Physical Therapy, Orthopaedics and Spine Medicine. Treatments including steroids, muscle relaxants and pain medications offered no improvement.
Upon further investigation, the patient was diagnosed with thoracic outlet syndrome (TOS), which was confirmed by ultrasound as well as by nerve block testing performed by Benjamin Abraham, MD, a specialist in Anesthesiology & Pain Management. A Cleveland Clinic vascular surgeon performed a right first rib decompression, anterior and middle scalenectomy. At the patient’s one-month follow-up, she reported being pain-free.
The case illustrates the role that pain specialists can play in diagnosing and treating TOS, a group of disorders involving constriction of nerves and/or blood vessels within the thoracic outlet. Compression of the neurovascular bundle may be caused by a wide variety of conditions, including the presence of a cervical rib, tumor, previous trauma, or repetitive motion injury related to work, sports or hobbies.
Symptoms can include pain, numbness and paresthesia in the shoulder, upper chest and arm, sometimes extending to the hands and fingers.
About 90% of TOS cases are neurogenic (nTOS), in which bone or soft tissue compresses thoracic nerve bundles. The venous subtype (vTOS) is caused by compression of the subclavian vein, which leads to swelling and pain. Arterial TOS (aTOS), the rarest and potentially most dangerous, involves compression of the subclavian artery. It can cause limb-threatening effects, including aneurysm with thrombosis and embolization.
Advertisement
Surgery is usually called for in vTOS and aTOS cases, but nTOS often can be managed with conservative interventions.
“We see a lot of patients with relatively mild neurogenic TOS symptoms that can be managed with either physical therapy or medications aimed at stabilizing the nerve,” says Dr. Abraham. “In some cases, once the patient has diagnostic answers, they want to work on position changes.”
Patients with TOS typically are referred to pain management from their primary care doctor, physical medicine specialist or a spine surgeon. In many cases, vascular specialists refer suspected nTOS patients to anesthesiology to help inform surgical decision making.
Clinical examination includes having the patient abduct their arms; in TOS patients, this will cause or increase numbness, tingling and sometimes loss of color. Medical history is important as well, as it may reveal relevant experience of chest or neck trauma or activities that involve repetitive movements that may be causing compression.
“The second part of the diagnosis includes blocking the anterior scalene muscle and sometimes the pectoralis minor muscle to see if relaxation of these structures relieves the thoracic outlet syndrome pain,” says Dr. Abraham. “If it does, then there’s some good evidence to suggest that the patient should proceed with an operation.”
In a subset of patients, there may be overlap between TOS and complex regional pain syndrome, Dr. Abraham explains.
“Part of what we’re doing is trying to differentiate: Is this a patient who really has thoracic outlet syndrome and is an operative candidate, or is this a patient with complex regional pain syndrome?”
Advertisement
Once the block has been performed, patient response is gauged through a pain diary or a verbal report.
“The old practice was that if a patient’s test shows that these structures were being impinged upon – either the nerve, artery or vein – they would automatically undergo surgery,” says Dr. Abraham. “That’s still the practice in many hospitals.”
At Cleveland Clinic, however, physicians from a variety of surgical disciplines seek non-surgical options where they make sense, and strive to maximize predictability of surgical outcomes. “Anesthesiology has had a long collaboration with spine surgeons, using selective nerve root block or a diagnostic blockade to identify the pain generator,” says Dr. Abraham. “Now that has carried over into vascular surgery.”
Within pain management, successful treatment is defined as functional restoration.
For some patients with TOS, the pain is not debilitating, says Dr. Abraham.
“But for many of the patients that we see in Pain Management, what we call the EAST maneuver (elevated arm stress test) – the hands-up/surrender motion you think of from the movies – is really a motion that these patients have to do in their day-to-day lives,” he says. “It’s provocative for this condition. If you’re an electrician and a lot of your job entails overhead work, you might be completely debilitated by this condition. That’s where the difficulty is.”
Cross-disciplinary work with these TOS patients can help restore a better quality of life.
“Neurogenic TOS is often a diagnostic dilemma, particularly when there are other confounding diagnoses. In these cases, a scalene block performed by the pain management team not only help confirm the diagnosis, but also determine how much relief a patient can expect from surgical intervention,” says vascular surgeon David Laczynski, MD. “When the correct diagnosis is made, patients can expect to be near or completely pain free after recovering from surgery in the vast majority of cases.”
Advertisement
Advertisement
Multidisciplinary perspectives on the importance of early referral and more
Findings could help with management of a common, dose-limiting side effect
Novel therapy “retrains” the brain to disrupt pain signals
Compassion, communication and critical thinking are key
Add AI to the list of tools expected to advance care for pain patients
Cleveland Clinic study investigated standard regimen
Despite the condition’s debilitating, electric shock-like pain, treatment options are better than ever
Program participation correlates with reduced use of opioids, X-rays and ED visits