New findings could shape the treatment paradigm for a select group of bladder cancer patients
Findings from a new Cleveland Clinic-led study help clarify the role of neoadjuvant chemotherapy in the management of bladder cancer with variant histology. Researchers presented these data at the 2021 American Urological Association meeting.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The prognosis for variant histology is generally worse than that of pure urothelial carcinoma. The treatment paradigm for the latter includes neoadjuvant chemotherapy with cisplatin followed by radical cystectomy. Treatment for non-muscle invasive bladder cancer with variant histology favors an aggressive therapeutic approach, progressing to radical cystectomy as a first-line therapy and bypassing neoadjuvant treatment altogether.
For patients with muscle-invasive bladder cancer with variant histology (with the exception of small cell carcinoma), the use of neoadjuvant treatment is unclear.
Rebecca Campbell, MD, a resident in Cleveland Clinic’s Glickman Urological & Kidney Institute and first author of the study, says this ambiguity led to a multi-institutional collaboration with colleagues at Mayo Clinic that helped jumpstart this investigation and others.
“These histologies are very rare and all previous literature comes from small single-institution series.”
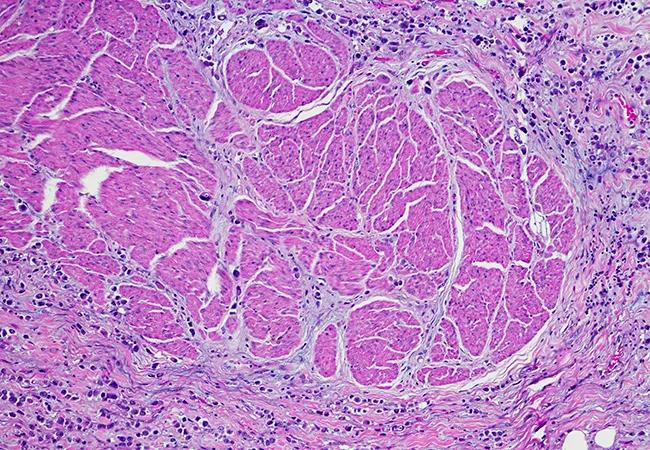
Together the teams partnered to create a larger database of patients with variant histology undergoing radical cystectomy than has previously been reported. They decided which histologies to include – urothelial, sarcomatoid, small cell carcinoma, nested, micropapillary and plasmacytoid – and determined pathologic downstaging after neoadjuvant chemotherapy would be a clinically meaningful endpoint.
“Downstaging occurred if the pathologic tumor stage at the time of radical cystectomy was lower than the clinical tumor stage, established at the time of transurethral resection of the bladder tumor,” she explains.
Advertisement
Their analysis included 889 patients, 303 with variant histology and 586 non-variant histology patients, all of whom underwent radical cystectomy from 1980 to 2018. Patients with variant histology were matched with pure urothelial carcinoma patients by age, sex, clinical tumor and nodal stages, year of radical cystectomy and receipt of the neoadjuvant chemotherapy.
“Our primary finding is that patients with variant histology can respond to neoadjuvant chemotherapy, demonstrated by pathologic downstaging,” Dr. Campbell says.
“Patients with pure urothelial carcinoma showed pathologic downstaging, which reinforces the role of neoadjuvant chemotherapy in their clinical management, and the matched variant histology cohort had strikingly similar rates.”
The rates of downstaging across variant histology subgroups varied, which should be considered, but Byron Lee, MD, PhD, senior author of the study and urologic oncologist in the Glickman Institute, says these findings provide a basis for broader integration of neoadjuvant therapy for this patient population going forward.
“This could mean potentially improving outcomes for select patients,” he says. “It answers some unknown questions in the management of these patients and opens the door for broader, multi-institutional collaborations to better understand this rare and comparatively aggressive pathology.”
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient