It’s time to get familiar with this emerging demyelinating disorder
Podcast content: This podcast is available to listen to online.
Listen to podcast online (https://www.buzzsprout.com/2243576/15385432)
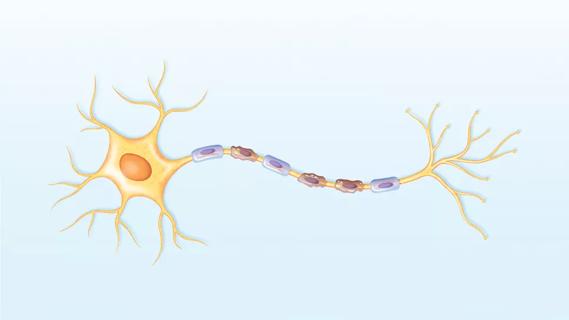
Myelin oligodendrocyte glycoprotein antibody disease (MOGAD) is a rare demyelinating disorder characterized by optic neuritis, myelitis, and inflammation of the spinal cord and brain. It primarily affects younger individuals and does not show a strong sex predominance.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“MOGAD is an emerging disease that general neurologists are likely to encounter more and more,” says Amy Kunchok, MD, PhD, staff neurologist in Cleveland Clinic’s Mellen Center for Multiple Sclerosis Treatment and Research. “It is more frequent than neuromyelitis optica spectrum disorder (NMOSD), and it’s a disorder to think about if you come across patients with optic neuritis, which is the most common presentation. When neurologists see this presentation or myelitis, they may want to think about referring to a tertiary center to arrange testing for MOGAD.”
In the latest episode of Cleveland Clinic’s Neuro Pathways podcast, Dr. Kunchok shares the essentials of MOGAD, covering the following:
Click the podcast player above to listen to the 20-minute episode now, or read on for a short edited excerpt. Check out more Neuro Pathways episodes at clevelandclinic.org/neuropodcast or wherever you get your podcasts.
This activity has been approved for AMA PRA Category 1 Credit™ and ANCC contact hours. After listening to the podcast, you can claim your credit here.
Podcast host Glen Stevens, DO, PhD: How does MOGAD differ from NMOSD, or neuromyelitis optica spectrum disorder?
Dr. Kunchok: There are several distinguishing clinical features as well as some paraclinical differences. From a clinical perspective, NMOSD and MOGAD both present with optic neuritis involvement, but the location for the inflammation of the optic nerve is different. It’s more anterior in MOGAD and more posterior in NMOSD. And in NMOSD it also often involves the chiasm. So there are some differences in anatomical involvement.
Advertisement
Dr. Stevens: You mentioned that in the spine you can have several segments affected in MOGAD, correct? But don’t you also see multiple segments in NMOSD?
Dr. Kunchok: Yes, for myelitis, both diseases do have longitudinally extensive lesions. So that is a similarity, but there are some differences. For example, there is less contrast enhancement for MOGAD, and we more often see T2 lesions confined to the gray matter. With NMOSD, we typically see contrast enhancement, sometimes an elongated ring of contrast enhancement, that is a classical feature for NMOSD.
The other distinguishing feature is that the lesions look quite different in the brainstem. Patients with NMOSD often have very discrete lesions. In particular, a classical feature for NMOSD is the area prostrema in the dorsal medulla, and patients will have intractable nausea and vomiting. In contrast, MOGAD patients will often have more diffuse, hazy lesions, sometimes involving the bilateral cerebellar peduncles. So these disorders have different imaging and clinical manifestations.
Dr. Stevens: What about MOGAD and MS? How are they similar and different?
Dr. Kunchok: In terms of optic neuritis, the main difference is that bilateral involvement is more common in MOGAD and unilateral is more common in MS. Again, the length of the lesion can be different. So MOGAD can have longitudinal extensive lesions of the optic nerve and MS can have short-segment lesions. Similarly, in the spinal cord, you might see longitudinal extensive lesions for MOGAD and short-segment lesions for MS. And on the axial segment you can see more centrally located lesions for MOGAD and more peripherally located lesions for MS. Those seem to be the typical differences between the two.
Advertisement
Advertisement

Despite less overall volume loss than in MS and NMOSD, volumetric changes correlate with functional decline

From dryness to diagnosis
Early experience with the agents confirms findings from clinical trials

Despite advancements, care for this rare autoimmune disease is too complex to go it alone
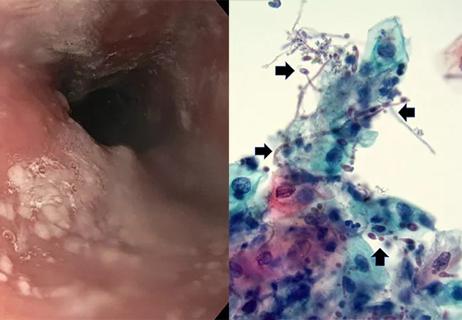
Treatment for scleroderma can sometimes cause esophageal symptoms
Patient’s symptoms included periorbital edema, fevers, weight loss

Could the virus have caused the condition or triggered previously undiagnosed disease?
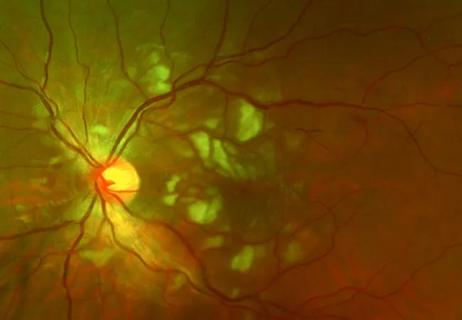
Good visual recovery and retinal reperfusion after prompt diagnosis and intensive therapy