Eight top trends to watch
What trends in mechanical circulatory support and other heart failure care excite you the most these days? That’s the question Consult QD posed to two Cleveland Clinic heart failure leaders: Jerry Estep, MD, Section Head of Heart Failure and Transplantation, and Edward Soltesz, MD, MPH, Surgical Director of the George M. and Linda H. Kaufman Center for Heart Failure and Recovery. Their responses are recapped below.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A magnetically suspended pump made Abbott’s HeartMate 3™ left ventricular assist device (LVAD) a recent game changer. Improved blood flow through the pump virtually eliminated clot formation and significantly reduced strokes. The result is an LVAD with two-year survival rates approaching those of transplantation, according to the pivotal MOMENTUM 3 trial.
Dr. Estep, a MOMENTUM 3 co-investigator who co-chaired the study’s Flow Optimization Subcommittee, says this is only the beginning of changes in LVAD design. These will include a pump that automatically regulates its speed to enhance functional capacity and quality of life, a key factor in hemodynamics that defines congestive heart failure.
He also expects LVADs to become fully implantable, lowering the risk of infection from holes in the skin.
Dr. Soltesz says this possibility is nearing reality. “We are looking at a transcutaneous energy transmission system, or TETS, that would allow an LVAD or other device to be charged through the skin,” he says.
Both specialists also foresee increased miniaturization and greater hemocompatibility to further reduce gastrointestinal bleeding, infection and stroke risks.
As LVADs challenge transplantation as the standard of care for advanced heart failure, new benchmarks for LVAD appropriateness are needed. The landmark ROADMAP trial has been a step forward, says Dr. Estep, who served as ROADMAP’s national principal investigator. “This trial provided an objective measurement of the risk/benefit ratio that’s helping us determine who should receive an LVAD,” he says. “It showed that the ideal patient is less sick than what traditional criteria had called for.”
Patient and caregiver understanding of LVAD benefits and risks is key, Dr. Estep adds. He served as a senior investigator in the VAD Decision Aid (VADDA) trial, which showed that this tool helps patients and their significant others be better informed in LVAD decision-making. The decision aid is available online and is routinely offered at Cleveland Clinic in addition to standard-of-care LVAD education.
As one of few centers with a comprehensive, multidisciplinary program of research and clinical care in heart failure, Cleveland Clinic has been involved in all major LVAD trials and developed a large database for outcome analyses designed to establish best practices. Current efforts aim to streamline care processes to speed recovery and reduce pain and its sequelae.
Minimally invasive LVAD implantation is one option being studied, though the jury’s still out on whether the pain reduction is significant enough to justify the more complex surgical approach. Separately, a protocol to reduce opiate dependency in LVAD patients has proved successful and is ready for widespread adoption. The program coaches patients preoperatively on postoperative pain and how it will be managed. Today, few Cleveland Clinic patients with LVADs are discharged on opiates.
If one LVAD is good, can two be better? For patients with biventricular dysfunction, the answer appears to be yes. Cleveland Clinic is developing a protocol for implanting two permanent VADs in these patients — one to support the left ventricle and another for the right ventricle.
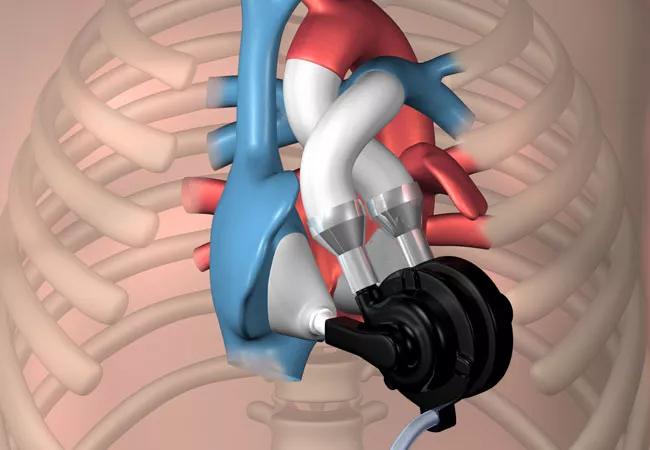
In the future, such patients may opt for the Cleveland Clinic continuous-flow total artificial heart (CFTAH), which is under development in adult and pediatric sizes. Its unique design (shown in illustration at top of post) has a circulating flow pump that rotates between right and left ventricles as it auto-regulates and balances blood flow. The device, currently in large-animal trials, is expected to move to human trials in the next few years.
Dr. Soltesz foresees development of durable versions of percutaneous devices like the Impella® that can be inserted in the axillary or femoral artery for temporary circulatory support. These new pumps will be durable enough to last several months and can be worn at home while patients await transplant.
When a heart struggles to recover after open-heart surgery, temporary use of a mechanical support device like the Impella can ease recovery. “We’ve found that supporting a poorly functioning heart for two or three days makes a significant difference,” says Dr. Soltesz. “If the heart doesn’t recover, we move toward LVAD implantation.”
Tafamidis is the first drug to show benefit in patients with transthyretin (TTR) amyloid cardiomyopathy. In the recent phase 3 ATTR-ACT study, tafamidis significantly reduced all-cause mortality and cardiovascular-related hospitalizations relative to placebo over 30 months. Cleveland Clinic’s Amyloidosis Center is engaged in additional investigator-initiated and multicenter clinical trials related to the diagnosis and treatment of TTR and AL amyloidosis, both of which are associated with progressive heart failure and have traditionally been resistant to therapy.
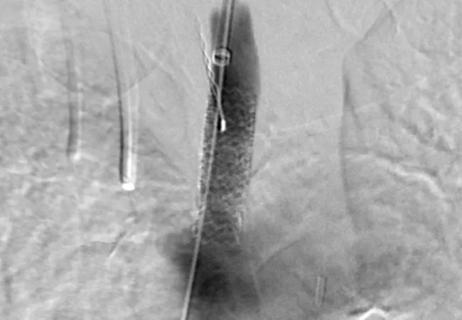
Remote hemodynamic monitoring with the CardioMEMS™ device reduces hospital readmissions while improving quality of life. The wireless pulmonary artery pressure sensor allows providers to monitor and guide treatment for patients who are at home.
Based on positive initial experience, Cleveland Clinic is participating in the multicenter GUIDE-HF trial to evaluate the effectiveness of CardioMEMS in a broader spectrum of patients. “We plan to implement use of this device at the system level to curb heart failure morbidity in patients with both reduced and preserved ejection fraction,” explains Dr. Estep.
Conducting one-week post-discharge visits online via virtual visits, rather than in person, also may reduce poor outcomes in heart failure patients following hospital discharge. Cleveland Clinic is leading a study evaluating whether virtual visits improve adherence to appointments and improve outcomes. Trial completion is expected in 2019.
How our first century has impacted cardiovascular practice

Review offers comprehensive assessment of the landscape for wearables and more

Preserving trust in research requires vigilance and consensus around statistical nuances

Cardiac surgeon Patrick Vargo, MD, reflects on his first year as Cleveland Clinic staff

Improved risk prediction for patients is at the heart of Dr. Aaron Weiss’ research interests

Centralization would likely bring better outcomes, experts say, but may not be feasible
Dr. Daniel Burns on mentorship, robotic valve surgery, statistics and more
JACC review makes the case and outlines how to ensure oversight