Preoperative Impella 5.5 placement can provide a critical safety net for high-risk patients
Often, patients with low ventricular ejection fraction are in need of conventional cardiac surgery but are denied the opportunity. Surgeons may be reluctant to operate because of the risk of postcardiotomy cardiogenic shock, which often requires treatment with high-dose inotropic and vasopressor medications and the use of advanced mechanical support. Despite such measures, cardiogenic shock in this setting is often fatal in the first few postoperative days.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
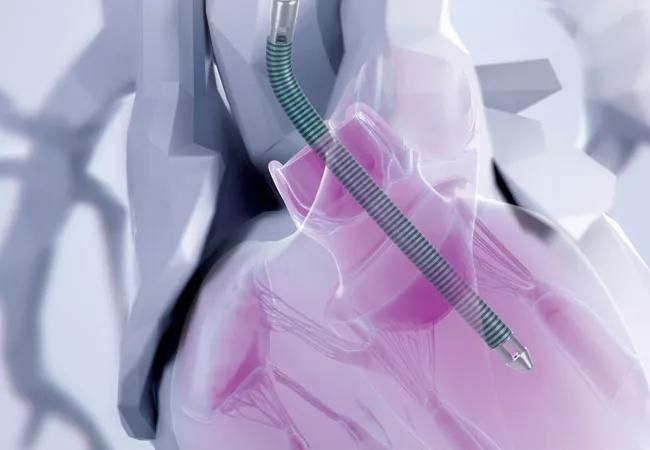
With the goal of expanding treatment options for patients at high risk of cardiogenic shock who are in need of coronary artery bypass grafting (CABG) or valvular surgery, Cleveland Clinic surgeons are preemptively employing the Impella 5.5 — a microaxial temporary left ventricular assist device (LVAD) — in selected patients. The device has several advantages over an intra-aortic balloon pump or extracorporeal membrane oxygenation. It can provide full left ventricular support for up to 14 days and allows patients to ambulate and recover while the heart is unloaded and supported. The Impella 5.5 is currently FDA-approved for cardiogenic shock after cardiac surgery or acute myocardial infarction.
“Patients with a low ejection fraction potentially benefit most from CABG or valve repair, so we are trying to make these procedures safer for them,” says Edward Soltesz, MD, MPH, Surgical Director at Cleveland Clinic’s Kaufman Center for Heart Failure Treatment and Recovery. “In our more than five years of experience employing preemptive Impella support, we have found that it leads to much better outcomes than reactive support.”
Use of advanced mechanical circulatory support can be a lifesaving measure, but it also entails risk of serious and even fatal complications, including myocardial puncture, thromboembolism and limb ischemia. Conventional thinking is to not use it for surgical patients until it is needed postoperatively. However, evidence indicates that mechanical support after postcardiotomy cardiogenic shock has developed is associated with high mortality, while preoperative or intraoperative mechanical support offers long-term survival similar to that of patients not requiring it.
Advertisement
Based on their experience, Cleveland Clinic surgeons have published several papers providing guidance on candidacy selection and management strategies for preemptive Impella use (Innovations.2021;16[3]227-230; Artif Organs. 2024;48:6-15; and Ann Thorac Surg. [Epub 2024 Feb 9]). They stress the importance of thorough coronary target and ischemic territory assessment, as well as myocardial viability and recovery potential.
“For patients with good targets, low scar burden and well-compensated heart failure, preemptive Impella placement is likely unnecessary,” says Michael Tong, MD, MBA, Director of Cardiac Transplantation and Mechanical Circulatory Support. “On the other end of the spectrum, very poor targets and extensive scarring are indicators of unlikely success of reparative surgery, and patients should be considered for heart transplantation or placement of a durable LVAD.”
“For patients with marginal targets and some increased scar tissue, we can be successful with preemptive mechanical support,” adds cardiac surgeon Faisal Bakaeen, MD. “Impella support is also an important strategy for patients with kidney or liver dysfunction, to maintain organ perfusion while buying time for the heart to recover.”
In a recent study in the Journal of Thoracic and Cardiovascular Surgery (JTCVS; Epub 2024 Mar 5), Cleveland Clinic surgeons reported on the use of random forest data analysis to assess potential risk factors of postcardiotomy cardiogenic shock. The following factors were identified to be highly associated with postcardiotomy cardiogenic shock:
Advertisement
“Identifying predictors of postcardiotomy cardiogenic shock helps us determine which patients are likely to benefit from preemptive Impella placement,” Dr. Soltesz adds. “Ultimately, however, it’s a judgment call based on our experience and on consideration of factors such as frailty and length of time the patient has been in intensive care.”
“We identified that the biggest predictor of how well a patient will tolerate the open-heart surgery is how well compensated they were going into surgery,” notes Dr. Tong.
This is an area where close collaboration with cardiologists, particularly advanced heart failure cardiologists, can be valuable, adds Amanda Vest, MBBS, MPH, Section Head of Heart Failure and Transplantation Cardiology. “Preoperative heart failure optimization can be key to a patient’s operative success, often through a combination of diuresis, optimization of medical therapies or, in some cases, utilizing temporary mechanical circulatory support to improve a patient’s hemodynamics before the surgery,” she says.
Cleveland Clinic surgeons emphasize that once the decision is made to pursue a strategy of preemptive Impella use, patients are best managed with thorough preoperative assessment, well-timed intervention and perioperative optimization.
Postoperatively, they aim for early extubation and ambulation. They advise gradual Impella withdrawal by turning down the device by one to two power levels daily, as tolerated. In most cases, the device can be removed four days postoperatively. Weaning and removal should be guided by hemodynamic improvement rather than echocardiographic changes, which manifest more slowly.
Advertisement
The surgeons also emphasize having planned exit strategies if a patient cannot be weaned from the Impella. For particularly high-risk patients, they recommend preoperative evaluation for heart transplantation or durable LVAD placement so that such options can be pursued if needed. “Our heart failure consultation team routinely meets with patients with low ejection fraction prior to their surgery,” Dr. Vest notes, “to determine their wishes and scope to benefit from a transplant or durable LVAD should the postoperative course require these considerations.”
Preemptive use of the Impella 5.5 is currently undergoing investigation in the multicenter, prospective, single-arm Impella-Protected Cardiac Surgery Trial (IMPACT; NCT05529654), which is enrolling 100 patients with low ejection fraction who will undergo CABG and/or valve replacement or repair. Dr. Soltesz is national co-principal investigator of the trial, which is expected to be completed in late 2025.
“We have had excellent outcomes with preemptive Impella placement for selected patients who currently are usually passed over for surgery,” Dr. Soltesz notes. “It is our hope that clinical trials will replicate our experience and lead to the addition of more indications for use of this strategy to increase treatment options for patients with heart failure.”
Drs. Soltesz, Tong and Bakaeen all underscore the importance of extensive experience with surgical treatment of patients with poor heart function in order to achieve good outcomes with this strategy. An expert multidisciplinary team is critical, they note, not only for determining a treatment strategy, but also for preoperative assessment and optimization, intraoperative technique and management of recovery.
Advertisement
“It’s this comprehensive approach to patients with low ejection fraction that has yielded the greatest benefit with minimal risk,” Dr. Tong says. “In our recent study in JTCVS, we operated on 238 consecutive patients between 2017 to 2020 with an ejection fraction below 30%. The mortality in this group of very sick patients was only 1.7%. Most notably, the mean ejection fraction in this group improved from 25% preoperatively to 39% at 12 months after surgery.”
“These patients tend to be complex, with a different risk profile than is typically encountered in hospitals with less volume-based experience,” adds Dr. Bakaeen. “Rather than passing over these high-risk patients, we highly recommend referral to a high-volume tertiary center for evaluation and treatment.”
Advertisement

Medical and surgical perspectives on current and emerging uses of ECMO and Impella

Least-invasive open-heart AVR option to date yielded rapid recovery in all cases

Launch of the tool promises to reshape quality assessment across the specialty

Lead dwell time and manufacturer emerge as independent predictors of success in registry study

The case for a thoughtful approach to CTO and minimally invasive options for CABG

How the tool could help physicians alter management in real time
Technique may lay groundwork for personalized decision-making in procedural intervention
Check out our latest volume and outcomes data in these key areas