Aortic valve replacement is best option for lowering mortality in this high-risk population
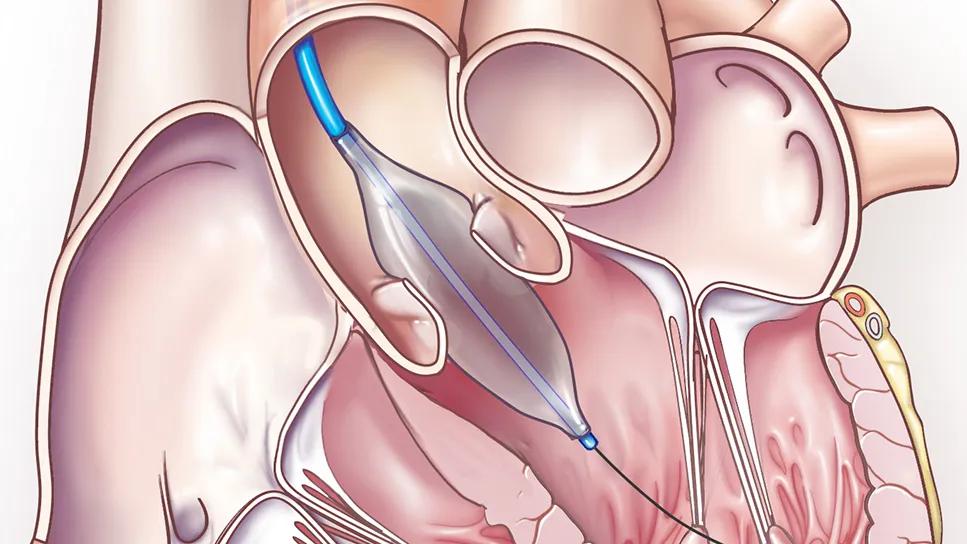
High in-hospital and 30-day mortality is common for patients with cardiogenic shock due to severe aortic stenosis (AS-CS), particularly with medical management. Balloon aortic valvuloplasty (BAV) lowers the risk, but only in the short term, whereas surgical and transcatheter aortic valve replacement (SAVR and TAVR) yield more-enduring benefit. So finds a retrospective Cleveland Clinic study evaluating the impact of these therapeutic approaches on the incidence and outcomes of AS-CS (J Am Heart Assoc.2024;13:e033601).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Our analysis suggests that adopting a lower threshold for aortic valve replacement may be key to improving survival in patients with cardiogenic shock due to aortic stenosis,” says Cleveland Clinic interventional cardiologist Grant Reed, MD, MSc, the study’s senior author. “Mortality rises to 50% in this population if balloon aortic valvuloplasty is not followed by definitive valve replacement within 90 days.”
“Cardiogenic shock due to aortic stenosis is associated with extremely poor outcomes, and treatment is challenging because data on which to base therapy selection are lacking,” says study co-author Venu Menon, MD, who directs the cardiac intensive care unit on Cleveland Clinic’s main campus. He notes that no guidelines exist for the management of AS-CS.
TAVR is standard of care for high-risk patients with severe aortic stenosis, but no patients with cardiogenic shock were included in randomized clinical trials of the procedure. The few studies of TAVR for cardiogenic shock in the literature lack treatment comparisons, and some were underpowered because of small cohort size. Research is likewise needed on BAV and SAVR in patients with AS-CS, and few comparisons have been done between surgical and transcatheter treatment in this setting.
To help fill those knowledge gaps, the authors analyzed data from 2,737 adults admitted to Cleveland Clinic’s cardiac intensive care unit with cardiogenic shock from 2010 through 2021. Of these patients, 199 (7.3%) had AS-CS.
Among the AS-CS patients, 81 (41%) received medical management, 70 (35%) received transcatheter therapies (BAV in 46 and TAVR in 24), and 48 (24%) underwent urgent SAVR.
Advertisement
The primary outcome, all-cause mortality at 30 days, was significantly higher among patients with AS-CS than among those with cardiogenic shock alone (30% vs. 20%; P = .0011).
Among patients with AS-CS, 30-day mortality was significantly higher in those managed medically (50%) than in those who received transcatheter or surgical therapy (18% and 16%, respectively) (P < .001).
Among AS-CS patients who received transcatheter therapies, in-hospital death was not significantly different between those who underwent TAVR versus BAV. By 30 days, however, mortality began to significantly diverge, reaching 26% with BAV versus 4% with TAVR (P = .04). Mortality with BAV rose to approximately 40% at 60 days and approximately 50% at 90 days, approaching the rate with medical management.
In multivariable regression analysis, after adjustment for other covariates, 30-day mortality was significantly elevated with medical management (hazard ratio [HR] = 3.69; 95% CI, 2.04-6.66) and significantly reduced with both transcatheter (HR = 0.30; 95% CI, 0.15-0.59) and surgical (HR = 0.23; 95% CI, 0.10-0.54) management.
Assessing adjusted all-cause mortality at one year, the authors found no significant difference in hazard ratios for medical management and BAV, whereas risk was significantly higher for medical management versus SAVR or TAVR (HR = 0.17 and 0.11, respectively; P <.0001 for both).
The authors observe that nearly 10% of admissions for cardiogenic shock also involve aortic stenosis and that patients with AS-CS will have a significantly higher risk of mortality, particularly if they receive medical management. BAV is beneficial, but only in the short term. The best short- and long-term outcomes can be achieved through definitive management with TAVR or SAVR.
Advertisement
“Clearly the effects of balloon aortic valvuloplasty diminish over time if it is not followed by more definitive management,” Dr. Reed notes.
He adds that since in-hospital mortality with BAV was comparable to that with TAVR and SAVR, BAV may be a reasonable first step for temporizing patients who are critically ill in whom SAVR and TAVR are contraindicated.
“This can be particularly helpful if the cause of cardiogenic shock is uncertain and it’s not clear if valve replacement would alter the treatment course,” Dr. Reed explains. “If the patient responds well and their underlying illness can be improved, then definitive valve replacement can be offered. This is the first study to provide time thresholds on the durability of balloon aortic valvuloplasty in patients with cardiogenic shock, which has been an elusive question to date. Our findings indicate that definitive valve replacement should be done as soon as possible, as over one-quarter of patients died within 30 days after valvuloplasty.”
“Aortic valve replacement is a highly effective treatment for cardiogenic shock due to aortic stenosis, as it relieves obstruction, offloads the left ventricle and restores forward flow,” adds Anthony Zaki, MD, a Cleveland Clinic cardiothoracic surgeon who was not involved in the study. “Correcting aortic stenosis results in a dramatic and immediate improvement in left ventricular ejection fraction and overall cardiac function, with patients deriving significant benefit from the intervention. While the decision for transcatheter versus surgical replacement is nuanced, surgery is unique in that it allows simultaneous correction of other commonly associated conditions, such as coronary artery disease, mitral regurgitation and atrial fibrillation.”
Advertisement
Advertisement

Cleveland Clinic research emphasizes taking a holistic and individualized approach to care of septic shock

Cleveland Clinic Abu Dhabi initiative reduces ICU admissions and strengthens caregiver collaboration

JACC State-of-the-Art Review details current knowledge and new developments

A new approach to care at Cleveland Clinic Martin Health Hospital highlights the value of LPNs in the acute care setting

Transport nurses prepare to manage all patients and acuity levels

AHA scientific statement outlines models for high-intensity staffing, specialized expertise and more

A scannable graphic recap of our latest data

Nursing Ethics Program provides education, encourages research and creates safe spaces for caregivers to receive support