Experts weigh in on the amyloid hypothesis and how to use lecanemab if approved
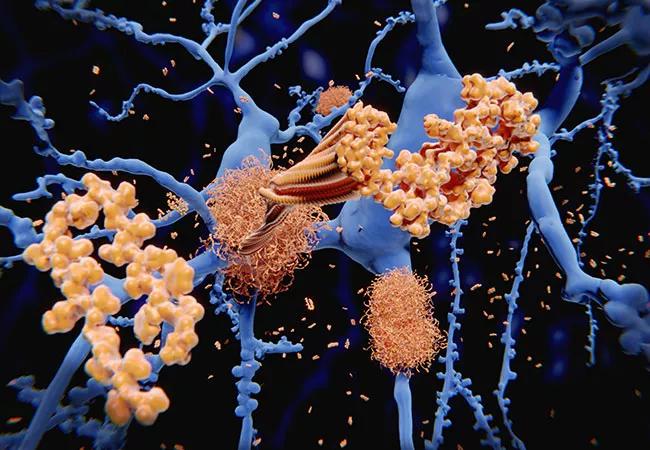
When results of the Clarity AD phase 3 clinical trial were published online in the New England Journal of Medicine in late November, the implications weren’t entirely clear, despite the “clarity” in the trial’s name. The double-blind, randomized study evaluated intravenous lecanemab (10 mg/kg of body weight every two weeks) versus placebo in 1,795 participants with symptoms of early Alzheimer’s disease (AD) and evidence of amyloid in cerebrospinal fluid or on PET. Lecanemab is a humanized monoclonal antibody targeting amyloid beta protein.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
At 18 months, the lecanemab cohort had less progression of clinical dementia than the control group, meeting the primary endpoint as measured by the Clinical Dementia Rating Sum of Boxes (CDR-SB) score. The difference between the groups in mean dementia progression was 0.45 points on the 18-point scale (P < 0.001). All key secondary endpoints that assessed cognition and function were also met, showing moderate but statistically significant reduction in decline in the intervention group compared with placebo.
Brain amyloid burden was evaluated by PET at baseline and 18 months in a substudy of 698 participants: the intervention group had a mean decrease of 55.48 centiloids versus an increase of 3.64 centiloids in the placebo group (P < 0.001).
Were the improvements seen with lecanemab clinically significant? How big of an issue was safety? And are researchers still on the right track by targeting amyloid for AD?
To gain some insight into these questions, Consult QD checked in with neurogeriatrician Babak Tousi, MD, who leads the clinical trials programs at Cleveland Clinic Lou Ruvo Center for Brain Health in Cleveland, and Charles Bernick, MD, Associate Medical Director of Cleveland Clinic Lou Ruvo Center for Brain Health in Las Vegas. Both sites participated in the Clarity AD trial.
Q: What do you make of Clarity AD’s findings? How meaningful is a 0.45-point difference in the primary endpoint?
Dr. Tousi: I’m not sure that’s the best way to look at it. Lecanemab clearly did what it was designed to do — it removed amyloid plaque. The results demonstrated all the downstream effects we hoped would happen in terms of reduction of biomarkers and less clinical decline on several functional and cognitive measures. So this difference will likely translate to a longer period of independent living for patients.
Advertisement
Dr. Bernick: The results are a confirmation of the idea that removing amyloid from the brain early in the disease process can slow disease progression. And it’s notable that the biomarkers, such as phosphorylated tau measures and amyloid measures in the blood, are all going in the right direction with lecanemab and some of the other anti-amyloid drugs. That adds credibility that these drugs are interfering with the disease process. In terms of how noticeable the slowed progression is, that may manifest more over longer follow-up than the current 18-month duration of this trial.
Q: The amyloid hypothesis — that removing amyloid plaque or preventing its deposition in the brain can slow or improve AD — has dominated the field for years. How have the results from this and other recent trials affected that thinking?
Dr. Bernick: Amyloid seems to be a trigger for a cascade of events leading to cell damage and cell death. The thought is that if you remove the amyloid trigger, there will be a positive impact on the disease process. The Clarity AD findings — and those for aducanumab, which is now FDA-approved for treating early AD – validate the amyloid hypothesis. Donanemab, another anti-amyloid drug, has also had encouraging phase 2 results for early symptomatic AD and is now undergoing a phase 3 trial and an open-label extension (TRAILBLAZER-ALZ 2; NCT04437511), with results expected in 2023.
There have also been trials of similar anti-amyloid drugs — gantenerumab, solanezumab and crenezumab — with disappointing findings. But there’s not enough information to determine why they didn’t appear to work as expected; there are so many factors at play. A failed drug trial doesn’t necessarily negate a hypothesis.
Advertisement
Dr. Tousi: I agree that the Clarity AD findings support the amyloid hypothesis and help justify the continued focus on anti-amyloid therapy for drug development. Keep in mind that the newly published results of Clarity AD were after only 18 months of treatment. The open-label extension phase will continue treatment and follow patients for up to 45 months (NCT03887455), so we can expect more answers.
Also important is determining whether the anti-amyloid drugs might be more effective when given earlier in the disease. To test this, Cleveland Clinic is involved in another critical placebo-controlled phase 3 trial — AHEAD 3-45 (NCT04468659) — which is examining the effect of lecanemab in patients with elevated amyloid but without clinical indications of Alzheimer’s. The trial is now recruiting and will follow participants through four years of treatment, with results expected in late 2027.
And I would add that amyloid is not the only target under investigation. Some kind of combination therapy might one day prove most effective. Perhaps anti-tau protein therapy – now in clinical trials – will prove to be a good adjunct to anti-amyloid therapy. Another potential target is inflammation.
Q: What about safety? In Clarity AD, amyloid-related imaging abnormalities (ARIAs) with edema or effusions occurred in 12.6% of the intervention group, and two deaths in the extension trial might be linked to these effects.
Dr. Bernick: These drugs clearly carry some risk, but Clarity AD taught us how to better choose candidates for therapy. Because ARIAs were likelier in carriers of the ApoE Ɛ4 allele, genetic testing should be used to screen potential candidates. Baseline brain MRIs are needed to rule out microscopic hemorrhages and other evidence of vascular disease. Patients taking blood thinners would likely also be disqualified. Most ARIAs arose soon after initiating the drug, so early close monitoring with MRI scans is indicated. Until we know more, MRI surveillance should continue throughout therapy. Patients with a cardiac defibrillator, who cannot undergo MRI scanning, would not be appropriate candidates.
Advertisement
Q: If lecanemab is approved by the FDA in the coming months as expected, will you recommend it to your patients?
Dr. Tousi: With the precautions outlined by Dr. Bernick, I would offer anti-amyloid therapy to patients who might benefit — that is, those who have early disease, are still independent and have evidence of amyloid. Otherwise, we do not know if it provides much benefit in advanced stages or is worth the risk associated with the therapy. And once a patient is on the drug, it’s important to reconsider risks and benefits as the disease progresses.
Doctors will need to educate patients and their families about what they can realistically expect from these drugs. Patients and families are desperate, and when they hear “Alzheimer’s treatment,” they want to give it a try. They need to understand that not everyone qualifies for treatment, and that people don’t get better on these drugs; they just decline more slowly.
Advertisement
Advertisement

An argument for clarifying the nomenclature

An expert talks through the benefits, limits and unresolved questions of an evolving technology

Recommendations on identifying and managing neurodevelopmental and related challenges

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits