GFAP elevation may signal increased risk of progressive regional atrophy, cognitive decline
Elevation of glial fibrillary acidic protein (GFAP) over time is correlated with volumetric losses in the brain and cognitive changes in individuals exposed to repetitive head impacts (RHI). So reveals a study assessing several blood biomarkers against brain imaging and cognitive findings among participants in Cleveland Clinic’s Professional Athletes Brain Health Study over an eight-year period. The findings were published in Alzheimer’s Research & Therapy (2023;15:173).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“As a longitudinal measure, plasma GFAP may have a role in identifying individuals at increased risk of progressive regional atrophy and cognitive decline, which suggests it ultimately might serve as an outcome measure in clinical trials,” says lead investigator Charles Bernick, MD, MPH, a staff neurologist with Cleveland Clinic Lou Ruvo Center for Brain Health in Las Vegas. “Measurements of neurofilament light chain, in contrast, appear to be more useful for reflecting neural injury in individuals actively exposed to repetitive head impacts.”
Begun in 2011, the Professional Athletes Brain Health Study is an ongoing longitudinal study of licensed mixed martial arts (MMA) fighters and boxers exposed to RHI. Participants undergo annual MRI and cognitive testing, as well as blood testing for GFAP, neurofilament light chain (NfL) and tau levels.
Data from the cohort have previously been used to assess the effects of RHI on brain structure over time, to inform criteria for traumatic encephalopathy syndrome and to assess the brain’s potential for repair after exposure to RHI.
In this analysis, four plasma biomarkers were examined:
In studies of traumatic brain injury, all four biomarkers have shown promise, but most of the reports have been limited by short follow-up periods, inclusion of participants exposed to only a single injury or use of limited outcome measures.
Advertisement
The primary aims of the current study were to assess the following:
The study involved 471 participants across four cohorts:
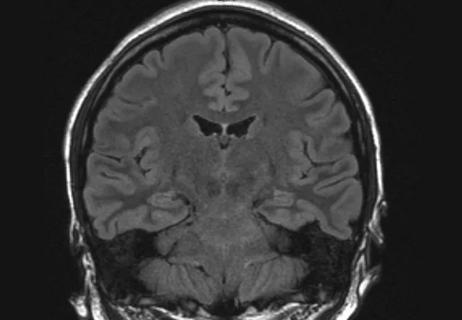
Data for the study were collected between 2011 and 2018. Baseline assessments included 3T MRI of the brain, plasma sampling and computerized cognitive testing (verbal memory, symbol digit coding, Stroop task and a finger-tapping test). Statistical analyses were performed to assess the relationship between plasma levels and regional brain volumes and cognitive performance at baseline and longitudinally.
Key findings related to the biomarkers studied were as follows:
Advertisement
The authors note that the increasing levels of GFAP in the retired boxers may reflect underlying neuroinflammation and/or astrogliosis as manifested by loss of regional volume and lower performance on cognitive measures. They also hypothesize that the increased NfL levels in the active boxers may reflect axonal injury from the many blows to the head the athletes typically sustain in training and competition.
“Monitoring plasma GFAP levels over time may help us identify people with prior repeated head impacts who are developing a neurodegenerative process,” Dr. Bernick says. “But without pathological confirmation, there is no way to truly know what type of pathophysiology the plasma GFAP represents.”
He cites this lack of pathological confirmation as the study’s primary limitation, with its strengths being its longitudinal comparison of biomarkers with imaging and cognitive measures in a large population with RHI exposure.
The authors conclude that additional longitudinal studies over longer periods and with additional RHI-exposed cohorts are needed to verify and refine their findings.
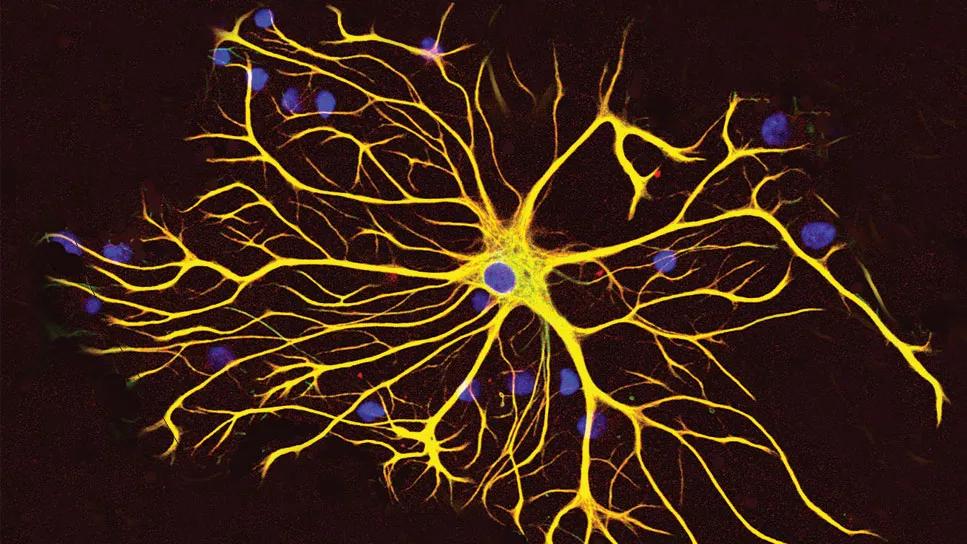
Image at top: An astrocyte cell grown in tissue culture stained with antibodies to GFAP and vimentin.
Image credit: GerryShaw, CC BY-SA 3.0, via Wikimedia Commons.
Advertisement
Advertisement
Diagnosis and treatment of MOG antibody-associated disease

Model of viral encephalomyelitis shows links with CNS recovery from inflammation and damage

Will enable sharper focus on new diagnostic tools for elusive neurodegenerative disease

New guidance on penetrating head injuries, and noninvasive diagnostics get a nod in austere settings

Novel insights from a postmortem study combining imaging, pathology and clinical perspectives

A principal investigator of the landmark longitudinal study shares interesting observations to date

Modest research progress to date can still be turned into meaningful patient gains

MRI classifier identifies a subset of patients with disease marked by cortical atrophy, not demyelination