Orthopaedic surgeons share insight on a recent clinical case

By Nicolas S. Piuzzi, MD, Hiba K. Anis, MD and George F. Muschler, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 45-year-old woman with a history of multiple organ transplants presented with a one-month history of anterior left hip pain with insidious onset. Although she was able to perform activities of daily living, she reported increasing difficulty with weight-bearing activities. Physical examination of the left hip elicited pain on passive movement, particularly on internal rotation. Plain radiography of the left hip (Figure 1) revealed a subchondral radiolucent line in the femoral head, representing subchondral collapse. This radiographic sign, referred to as the “crescent sign,” is seen in advanced stages of osteonecrosis of the femoral head. Recognition of this subtle radiographic sign is important because it represents considerable subchondral necrosis and collapse, and indicates that further collapse is likely¹.
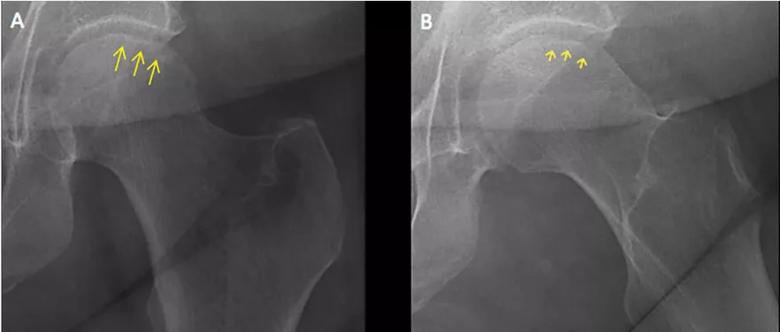
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0819ef1d-3dab-48b2-9ff7-446a457154e0/19-ORT-1343-Hip-Pain-CQD-F1_jpg)
Figure 1. Plain radiography of the left hip reveals a subchondral radiolucent line in the femoral head, representing subchondral collapse
Osteonecrosis of the hip is caused by prolonged interruption of blood flow to the femoral head.² While idiopathic osteonecrosis is not uncommon, the condition is often associated with alcohol abuse or, as in our patient, long-term corticosteroid use after organ transplant.³ Corticosteroid use is also the most frequently reported risk factor for multifocal osteonecrosis. Less common risk factors include systemic lupus erythematosus, antiphospholipid antibodies, coagulopathies, sickle cell disease, Gaucher disease, trauma, and external-beam therapy. Young age is also associated with osteonecrosis, as nearly 75% of patients are between age 30 and 60.⁴
Advertisement
Our patient had a typical clinical presentation of this disease: she was relatively young, was on long-term corticosteroids, and had acute anterior groin pain followed by progressive functional impairment. The diagnostic evaluation consists of a detailed history, with attention to specific risk factors, and a thorough clinical examination followed by imaging, usually with plain radiography. However, plain radiographs are often unremarkable when the condition is in the early stages. In such cases, magnetic resonance imaging is recommended if clinical suspicion for osteonecrosis is high. It is far more sensitive (> 99%) and specific (> 99%) than plain radiography, and it detects early changes in the femoral head such as focal lesions and bone marrow edema.⁵
Treatment of osteonecrosis is surgical and depends on the stage of disease.⁶ Joint preservation may be an option for small to medium-sized lesions before subchondral collapse has occurred; options include core decompression, bone grafting, and femoral osteotomy to preserve the native femoral head. These procedures have a higher success rate in young patients. Subchondral collapse usually warrants hip replacement.
Our patient underwent total arthroplasty of the left hip. Macroscopic inspection and palpation of the femoral head demonstrated chondral softening. Anatomic specimens (Figure 2) showed the distinct correlation between radiographic images and subchondral collapse secondary to the underlying necrotic bone in the femoral head.
Advertisement
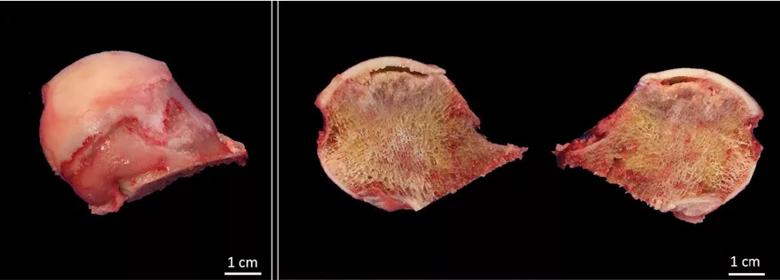
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/cedc9253-d182-4042-98bb-eb9ee280cb3d/19-ORT-1343-Hip-Pain-CQD-F2_jpg)
Figure 2. Anatomic specimens show distinct correlation between radiographic images and subchondral collapse secondary to the underlying necrotic bone in the femoral head.
This article is reprinted from Cleveland Clinic Journal of Medicine (2019; 86:511-512).
Dr. Piuzzi is associate staff, Adult Joint Reconstruction in the Department of Orthopaedic Surgery.
Dr. Anis is a research fellow in the Department of Orthopaedic Surgery
Dr. Muschler is staff in the Department of Orthopaedic Surgery and professor in Lerner College of Medicine of Case Western Reserve University.
Advertisement
Advertisement

How it’s similar but different from the direct anterior approach

Collaboration must cross borders and disciplines

Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols

Should surgeons forgo posterior and lateral approaches?

How chiropractors can reduce unnecessary imaging, lower costs and ease the burden on primary care clinicians

Why shifting away from delayed repairs in high-risk athletes could prevent long-term instability and improve outcomes

Multidisciplinary care can make arthroplasty a safe option even for patients with low ejection fraction

Percutaneous stabilization can increase mobility without disrupting cancer treatment