High-risk procedure prepares patient for lifesaving heart surgery
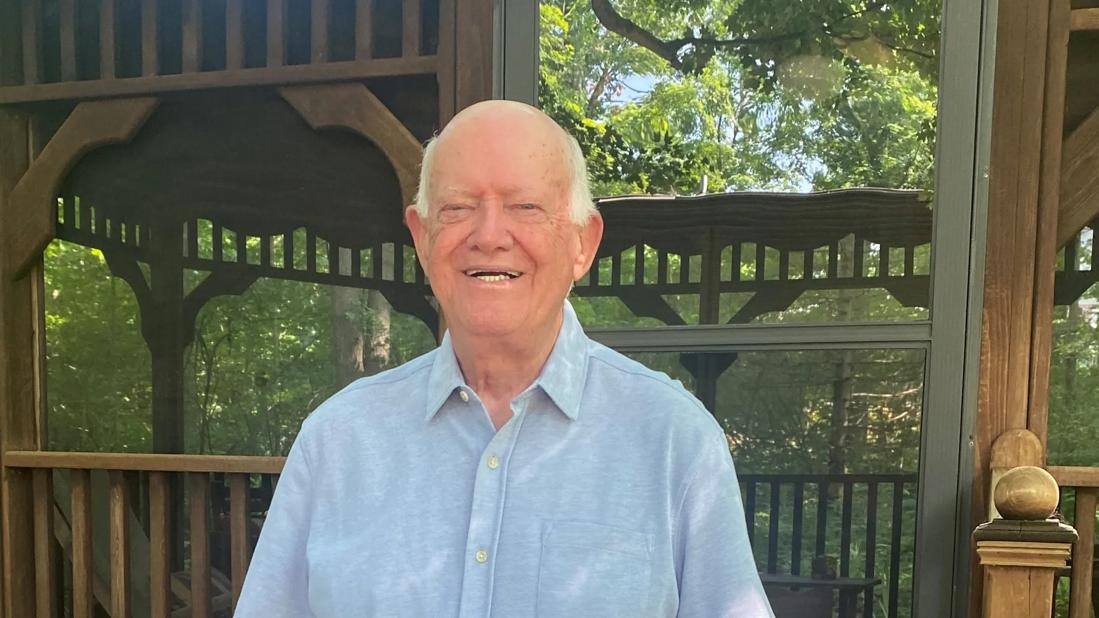
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1605ef40-30b6-4b02-bb9f-7c7a9fea9f71/randoll-7-r)
Patient who had hip revision and heart failure
“We did it again. It didn’t end in 2016 thanks to God, you and Cleveland Clinic.”
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
That’s the email message that Cleveland Clinic orthopaedic surgeon Nathan Mesko, MD, has received every Feb. 15 for the past eight years. It’s the birthday of a patient (pictured above) who, in 2016, had been admitted to Cleveland Clinic’s cardiac ICU with infective endocarditis that caused his heart valves to malfunction. The infection had become systemic and seeded his hip implant. In addition, the patient had two blocked arteries. His heart was working at less than 10% capacity.
To be a candidate for lifesaving heart surgery, the patient first needed to have his infected long-stem hip prosthesis removed — a four-to-five-hour surgery that would cause a large amount of blood loss and increased stress on his already-compromised heart.
“Every statistic indicated the patient likely would not survive the orthopaedic procedure,” Dr. Mesko says. “But the outlook would have been even worse if we did nothing. The only way to give the patient a chance at survival, by safely addressing his heart, was to remove his infected hip replacement. Along with the cardiac team, the patient and his family, we decided to go ahead with the high-risk operation.”
When the patient, then age 68, presented at Cleveland Clinic with heart failure, his dyspnea was so severe that he could not complete a sentence without taking multiple breaths. He was emergently intubated.
“We knew the infection began in the heart valves,” says cardiologist Steven Nissen, MD. “However, the hip infection needed to be cleared first so it wouldn’t reinfect the valves after heart surgery.”
Advertisement
The patient had been treated at an outside hospital that had attempted to eradicate the hip infection multiple times with simple debridement procedures, retaining the implants. The patient was taking multiple oral antibiotics. A draining sinus tract had been present for many months. Because conservative treatments had proven ineffective, hip revision surgery was the next step.
The challenge: Help the patient endure the complex orthopaedic operation with a weakened heart.
Revision is always more complex than primary arthroplasty, says Dr. Mesko.
“It’s complicated by scar tissue and anatomy that has been adulterated by prior surgery,” he says. “Getting into the joint is quick, but it takes a lot of time to remove a prosthesis that is well-healed to the bone while preserving as much bone as possible to accommodate a replacement revision prosthesis down the road. This case had additional complexity because of the patient’s heart health.”
The plan: Perform the hip revision arthroplasty in a cardiac operating room with a cardiac anesthesia team.
Before the procedure, Dr. Mesko gathered the 10-plus members of the surgical team — including a cardiac anesthesiologist and a cardiologist — to discuss exact steps and timing.
“It was like a symphony,” Dr. Mesko says. “We rehearsed it and then started the performance. Most straightforward surgeries are not orchestrated as precisely, but when it comes to complex, multidisciplinary operations, each individual needs to know their vital contribution. A major reason we were successful is because every caregiver knew their cue to step into the spotlight. It was a flawless performance.”
Advertisement
The cardiac team inserted a Swan-Ganz catheter to monitor the patient’s cardiac output, blood pressure and heart valve function throughout the procedure. Given the weakened state of the heart, the cardiac team needed to maintain a careful balance of fluid and medications to help the patient’s body accommodate the stresses of the operation. Additional resources, such as ECMO, were available to maintain heart function if needed.
The orthopaedic team performed an extended trochanteric osteotomy, a controlled fracture of the bone that involved using a clamshell technique to wedge open the femur, and removed the implant and infection. They then repaired the controlled fracture, removed the hip socket, debrided the joint, inserted a spacer and closed the wound.
“Usually, I try to remove the stem implant without a clamshell, but this time I didn’t have extra minutes to perform something simpler,” Dr. Mesko says. “Even though it was a slightly bigger surgery, it reduced the time that the heart was under added stress.”
After the 4.5-hour hip revision procedure, the patient went back to the cardiac ICU. His body was resuscitated, and four days later the patient returned to a cardiac operating room where he had three valve replacements, two bypasses and repair of a perforated septum.
He was discharged to a rehabilitation facility 30 days after his cardiac surgery. Six months later, he returned to Cleveland Clinic to have the hip spacer removed and receive a new hip prosthesis. He currently remains free of infection.
Advertisement
“We would never have recommended surgery if we didn’t think we could do it successfully,” Dr. Nissen says. “With excellent anesthesia, intraoperative and postoperative care, critically ill patients like this can survive very high-risk surgery.”
Years later, the patient continues to express thanks to the surgical team that wasn’t deterred by high risk and formidable challenge.
“Receiving his thank-you email each year is an annual reminder of the impact our multidisciplinary teams make, far beyond a single surgical or clinical encounter,” Dr. Mesko says. “A total team effort can make the impossible possible. The patient beat the odds. The email he sends every February reminds me of the incredible power that we have to restore life when all hope is lost.”
Advertisement
Advertisement
How it’s similar but different from the direct anterior approach
Should surgeons forgo posterior and lateral approaches?
Multidisciplinary care can make arthroplasty a safe option even for patients with low ejection fraction
Cleveland Clinic is among the first in the U.S. to perform the procedure
Insights to help orthopaedic practices comply with the 2025 CMS mandate
Dr. Piuzzi wins 2025 Kappa Delta Young Investigator Award for pioneering work
For patients with anatomic abnormalities, substantial bone loss and pre-existing hardware
How it actually compares to posterior and lateral approaches