19 in 20 will not have an allergic reaction
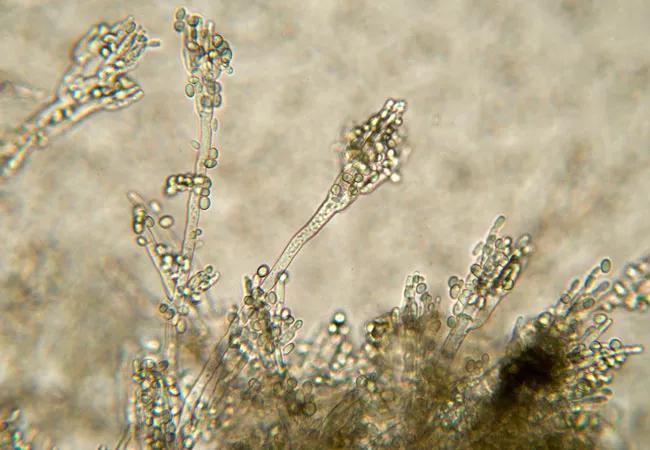
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/60cbe247-33d2-43e8-be6c-63ebb7410bf8/penicllium-mold_650x450_jpg)
penicllium-mold_650x450
Nearly 10 percent of the U.S. population self-reports an allergy to penicillin, thereby limiting their access to this effective antibiotic. But true IgE-mediated allergy to penicillin is uncommon. Moreover, evidence accumulated over the past decade and a half suggests that alternative antibiotics are less effective and cause more complications than penicillins.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The answer to this problem is simple: Verify the accuracy of this diagnosis before the patient requires another antibiotic.
“In our experience, 19 of 20 patients will be skin-test negative and able to tolerate penicillin without an adverse reaction,” says David Lang, MD, Chairman of the Department of Allergy and Immunology at Cleveland Clinic and President-elect of the American Academy of Allergy, Asthma, and Immunology (AAAAI).
Three reasons explain why the overwhelming majority of patients with a history of penicillin allergy will have negative skin tests, he says:
With concerns about the effects of inappropriate antibiotic use on antimicrobial resistance, the AAAAI, the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America looked into the issue. Their recent guidelines for evaluating patients for penicillin allergy are designed to help practitioners differentiate true allergic reactions from sensitivities and safely evaluate reported penicillin allergy. The guidelines delineate risk stratification for penicillin allergy evaluation.
Advertisement
Very low and low-risk patients include those reporting reactions that are unlikely to be allergic in nature, such as gastrointestinal symptoms, headache, sleepless nights or rash without pruritis, as well as family history of penicillin allergy.
Unknown reactions not compatible with an IgE mechanism that occurred more than 10 years prior also render a patient low-risk.
These patients may be prescribed a course of amoxicillin or challenge dose of amoxicillin under observation.
“Most people are in this category: They simply had an adverse experience that was never verified as a true allergic reaction and resulted in their being mislabeled with a penicillin allergy,” says Dr. Lang.
Patients considered at moderate pre-test probability for allergic reaction with re-exposure to a penicillin should be skin tested. If the skin testing is negative, an amoxicillin challenge under observation should follow.
“These patients may have reported cutaneous symptoms such as urticaria, pruritis, angioedema or flushing, or a reaction with features of IgE, but not anaphylaxis. Symptoms also may be respiratory, cardiovascular or gastrointestinal in nature,” says Dr. Lang.
Patients at high risk for penicillin allergy include those who experienced anaphylaxis, had reactions to multiple beta-lactam antibiotics or had a positive penicillin skin test. They should be referred to an allergist/immunologist for further evaluation.
The new, triple society-authored guidelines contain comprehensive detail on symptoms, procedures and contraindications to testing, along with the management of drug-challenge reactions. The information is designed to provide clinicians with the knowledge necessary to be comfortable moving ahead with evaluation of patients with unverified penicillin allergy.
Advertisement
“It is in the best interest of these patients to determine whether they are truly allergic to penicillin. If they are not, this opens the door to using a class of antimicrobial agents with fewer complications, while increasing the likelihood of a improved healthcare outcomes,” says Dr. Lang.
Advertisement
Advertisement
Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development
Recent breakthroughs have brought attention to a previously overlooked condition
A review of treatment options for patients who may not qualify for surgery
Looking at the real-world impact and the future pipeline of targeted therapies
The progressive training program aims to help clinicians improve patient care
New breakthroughs are shaping the future of COPD management and offering hope for challenging cases
Exploring the impact of chronic cough from daily life to innovative medical solutions
How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program