Measured rollout will tap the drug’s promise while navigating its complex REMS program

Cleveland Clinic will begin offering brexanolone, the first medication to treat moderate to severe postpartum depression, via a pilot program at one of its regional hospitals soon after the drug’s launch, which is expected in late June. The fast-acting neurosteroid, which received FDA approval in March under the name Zulresso™, is administered via continuous IV infusion for 60 hours in an inpatient setting.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
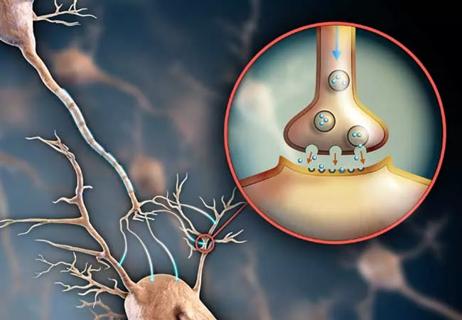
As detailed in this earlier Consult QD post, brexanolone is a derivative of endogenous allopregnanolone, a hormone that declines after childbirth. It works as an allosteric modulator of GABA-A receptors. GABA is an inhibitory neurotransmitter and may play an important role in modulating vulnerability to depression and anxiety.
“Brexanolone has the potential to change the treatment approach for postpartum depression and rapidly alleviate its adverse impact on mother, infant and family,” says Lilian Gonsalves, MD, Clinical Professor of Medicine at Cleveland Clinic Lerner College of Medicine and a staff physician in the Department of Psychiatry and Psychology. “Instead of waiting two to four weeks for a treatment response with traditional antidepressants, response with brexanolone takes two to four days. That’s phenomenal.”
“From a therapeutic viewpoint, we’re excited about brexanolone infusion because it represents a novel approach to treatment of postpartum depression,” adds Adele Viguera, MD, a Cleveland Clinic consultation-liaison staff psychiatrist and researcher in women’s mental health. “Our intention with this clinical pilot is to get some firsthand experience administering the drug and setting up a delivery system in one of our obstetrics centers.”
That effort is taking place via a brexanolone pilot program at Cleveland Clinic Hillcrest Hospital spearheaded by Cleveland Clinic consultation-liaison staff psychiatrist Lara Feldman, DO, and Sudhakar (Ken) Rao, MD, Director of Obstetrics at Hillcrest Hospital. They are modeling the program in adherence to FDA guidelines, most notably the inclusion of a Risk Evaluation and Mitigation Strategy (REMS) in view of the drug’s potential for severe sedative effects.
The brexanolone REMS requires that patients be under 24-hour supervision with monitoring by an on-site medical professional in a certified healthcare facility throughout the 60-hour continuous infusion. Continuous pulse oximetry must be administered, with an alarm for excessive sedation.
“Since the therapy can lead to excessive sedation, the REMS program is warranted,” says Dr. Feldman. “The last thing we want is to have a depressed, sedated mom caring for a newborn unsupervised.”
Obstetricians at Hillcrest Hospital routinely screen patients for postpartum depression using the 10-item Edinburgh Postnatal Depression Scale (EPDS) or the Patient Health Questionnaire (PHQ-9). A score ≥12 on the EPDS or ≥10 on the PHQ-9 triggers a referral to psychiatry, at which point Dr. Feldman or a psychiatrist colleague determines if the patient is a good candidate for brexanolone based on the severity of her symptoms.
Patients can receive treatment any time during the first year after giving birth, but the symptoms need to have started within the first six months postpartum.
Each woman who is eligible and consents to this treatment will be admitted to a postpartum unit, along with her baby (and a family member to watch the baby), and be followed by a psychiatrist. She will then receive the 60-hour infusion under the supervision of a trained nurse co-managed by a psychiatrist and obstetrician. One week after the patient is discharged, she will have a combined follow-up appointment with the psychiatrist and her obstetrician.
“We also plan to follow this treatment group with shared medical appointments for a year to monitor for relapse of symptoms,” Dr. Feldman notes.
After this pilot, if patient demand is sufficient, Cleveland Clinic may roll out the treatment to its other birthing centers in Northeast Ohio and perhaps additional regional sites.
As the psychiatry team prepares for Hillcrest Hospital to become one of the first facilities to offer brexanolone, they have several broad bits of advice for others who may follow them:
Dr. Feldman sees great potential for brexanolone therapy. “Postpartum depression has a deleterious effect on the mother/child bond and often on early child development and even long-term development,” she says. “Our hope is that brexanolone can quickly allow us to get moms healthy and able to care for their children. This could be a major breakthrough.”

Consultation service provides comprehensive care to patients with anxiety, PTSD, schizophrenia, and other high-risk disorders

Study shows a growing openness to the clinical potential of psychedelic treatments

Urine test strips and point-of-care testing may be key to slowing opioid epidemic

Study sheds light on how clinicians addressed their patients’ pain and insomnia during the pandemic

Recovery's in Reach provides treatment options, peer support to those struggling with alcohol and drug use

Experts recommend task-focused strategy for monitoring treatment
Finding changes the treatment landscape of psychiatric illness

Patients benefit when doctors disclose with care