Patient-derived model mirrors the disease’s complexity better than others currently available

A novel, patient-derived model of ulcerative colitis was used to identify a promising target that could be inhibited to slow the progression of chronic inflammatory bowel disease. The Cleveland Clinic researchers hope that their model will advance studies into new treatments for the chronic inflammatory bowel disease. Their work was reported recently in Nature Communications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
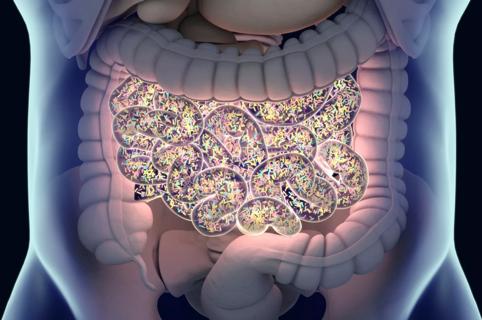
Ulcerative colitis is characterized by abnormal reactions of the immune system that lead to inflammation and ulcers on the inner lining of the large intestines. It is a highly heterogeneous condition, both in terms of patients’ symptoms and disease pathology.
Suppressing the overactive immune response with anti-inflammatory drugs is the current mainstay treatment for inflammatory bowel diseases, although these therapies have limited long-term efficacy in ulcerative colitis patients.
Research suggests that elements of both the immune system and the ulcerative colitis microenvironment (i.e., the surrounding, less diseased cellular components) interact to drive disease development and progression. Considering that immune-suppressing drugs have demonstrated limited success in treating ulcerative colitis, researchers are interested to learn whether targeting elements of the microenvironment — including components of the epithelium and stromal cells — may be a better or complementary treatment approach.
“Gaining a more comprehensive understanding of the complex interplay between immune and other cell types will be critical to developing new and more effective ulcerative colitis therapies and tailored, patient-specific treatment approaches,” said the study’s lead author Emina Huang, MD, of the Departments of Colorectal Surgery and Cancer Biology.
Dr. Huang and her team developed their model using tissue samples from patients with ulcerative colitis who underwent surgery at Cleveland Clinic. They isolated fibroblasts, which can be “reprogrammed” to develop into all-purpose, undifferentiated cells called induced pluripotent stem cells, which have emerged as a growing research priority.
Advertisement
The researchers then grew these stem cells in the lab into tiny, three-dimensional tissues that mimic actual organs (called organoids). They found that compared to healthy colon organoids, the diseased organoids reflected histological and functional features commonly observed in ulcerative colitis patients, including reduced mucus secretions, faulty barrier integrity of the intestinal lining and overexpression of select proteins (including one called CXCL8).
“Our in vitro model accurately mirrors what we observe in patients in the clinic and is much more dynamic than current models. For example, other organoid models only focus on the contributions of the epithelium, where ours reflects the contributions of other microenvironment components, too, like the stroma,” commented Dr. Huang.
After developing the model, the team was able to rapidly identify novel drug targets and candidates. They showed that inhibiting CXCL8 expression with a small molecule called repertaxin helped to slow disease progression.
“We look forward to further exploring repertaxin’s potential benefit in other preclinical and eventual clinical studies,” said Dr. Huang. “We are hopeful that others will also find this model useful in identifying other potential anti-ulcerative colitis drugs.” She also noted that the approach used to develop this new ulcerative colitis model may also be used to model other complex diseases.
Samaneh Sarvestani, PhD, a former research associate in Dr. Huang’s lab, is first author on the study, which was supported in part by the National Institutes of Health and the American Society of Colorectal Surgeons.
Advertisement
*Note: This article was originally published here.
Advertisement
Advertisement

First full characterization of kidney microbiome unlocks potential to prevent kidney stones

Researchers identify potential path to retaining chemo sensitivity
Large-scale joint study links elevated TMAO blood levels and chronic kidney disease risk over time

Investigators are developing a deep learning model to predict health outcomes in ICUs.

Preclinical work promises large-scale data with minimal bias to inform development of clinical tests

Cleveland Clinic researchers pursue answers on basic science and clinical fronts

Study suggests sex-specific pathways show potential for sex-specific therapeutic approaches

Cleveland Clinic launches Quantum Innovation Catalyzer Program to help start-up companies access advanced research technology