And why they matter, in the words of their investigators

Seven hundred seventy-seven. That’s the number of articles published in the peer-reviewed literature in 2017 by Cleveland Clinic Miller Family Heart & Vascular Institute staff, and the total for 2018 is on track to be comparable.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Leaders of the Heart & Vascular Institute looked back on their team’s hundreds of publications from 2018 to identify a handful that promise to be among the most noteworthy cardiovascular studies of the year. We profile 10 of those investigations here — and why they matter.
(N Engl J Med. 2018;379:2307-2318)
The multicenter COAPT trial found that transcatheter mitral valve repair with the MitraClip® device significantly reduced all-cause mortality and hospitalization compared with medical therapy in symptomatic patients with heart failure and secondary mitral regurgitation (MR). Benefits were consistent across multiple subgroups and were independent of MR grade and baseline left ventricular volume and function. The results are expected to lead to FDA approval of MitraClip for a new indication — treatment of secondary MR.
“This is the first large trial to show that treating functional MR not only makes patients feel better and prevents further worsening of the regurgitation, but also prevents death,” says Cleveland Clinic’s Samir Kapadia, MD, one of COAPT’s lead investigators and steering committee members. “It’s likely to change management of this high-risk patient population with symptomatic MR secondary to heart failure.”
“We have an important new option for patients with heart failure and severe functional MR,” adds Cleveland Clinic Cardiothoracic Surgery Chair A. Marc Gillinov, MD, who served on advisory and central eligibility committees for the trial. “Most of these patients are not good surgical candidates, but they can now receive a mitral procedure that improves their prognosis.”
Especially notable are the number-needed-to-treat results, Dr. Kapadia says: “We found that we need to treat just three patients to prevent one hospitalization and treat six patients to save a life. This is one of the most beneficial treatment effects we’ve ever observed in a clinical trial.”
(N Engl J Med. 2018;378:1386-1395)
This 69-center study showed that, among patients with advanced heart failure, the HeartMate 3™ fully magnetically levitated centrifugal flow pump was superior to the HeartMate II mechanical-bearing axial-flow pump in two-year survival free of disabling stroke or reoperation to replace/remove a malfunctioning device. Moreover, the HeartMate 3 was associated with a lower risk of stroke while averting device malfunction related to pump thrombosis.
“Two-year survival with the HeartMate 3 approaches that of heart transplantation,” observes Cleveland Clinic Heart Failure Section Head Jerry Estep, MD, who served as a leading MOMENTUM 3 co-investigator and co-chair of its flow optimization subcommittee. “This study was a tremendous opportunity to better understand hemocompatibility and the interaction between pump speed adjustments and medical management to optimize hemodynamics to improve patient outcome.” He adds that HeartMate 3 represents only the beginning of a budding evolution in left ventricular assist device (LVAD) design, which he says will include a pump with speed auto-regulation to enhance functional capacity and quality of life.
A novel imaging biomarker that quantifies perivascular fat can predict all-cause and cardiac mortality above and beyond clinical risk factors and current coronary CT interpretation methods. So found this cross-continental collaboration between UK researchers and colleagues in Germany and at Cleveland Clinic. High values of the biomarker — known as the perivascular fat attenuation index — around the right coronary artery effectively identified individuals at risk of death in two large, independent and substantially different patient cohorts: a derivation cohort in Erlangen, Germany (N = 1,872), and a validation cohort at Cleveland Clinic (N = 2,040).
“The perivascular fat attenuation index is the first noninvasive biomarker of coronary inflammation measured by traditional coronary CT angiography,” says co-first author Milind Desai, MD, a Cleveland Clinic cardiologist. “Our study validates the prognostic role of this index over and above the presence of coronary stenosis or calcification. We now have, for the first time, a biomarker derived from a fairly routine imaging study that measures residual cardiovascular risk with independent and incremental value over modern risk scores and other noninvasive tests. This could have transformative effects on primary and secondary prevention.”
(JAMA Netw Open. 2018;1(6):e183605)
Cardiorespiratory fitness is associated with long-term mortality benefits in a dose-response manner that shows no upper limit, according to the largest-ever cohort study of long-term mortality among patients undergoing exercise treadmill testing. “Extremely high aerobic fitness was associated with the greatest survival, and this benefit extended to individuals aged 70 or older,” says co-author and Cleveland Clinic cardiologist Wael Jaber, MD.
The retrospective cohort study included consecutive adults referred for symptom-limited exercise treadmill testing at Cleveland Clinic from 1991 through 2014. Median follow-up was 8.4 years. Based on their treadmill tests, patients were stratified by age- and sex-matched cardiorespiratory fitness levels into five performance groups: low (< 25th percentile), below average (25th-49th percentile), above average (50th-74th percentile), high (75th-97.6th percentile) and elite (≥ 97.7th percentile).
Risk-adjusted all-cause mortality was found to be inversely proportional to cardiorespiratory fitness, with statistically significant differences between each increment in fitness level. Elite fitness was associated with an 80 percent reduction in mortality risk relative to low fitness. The mortality increase associated with each reduction in fitness level was comparable to or greater than that of traditional clinical risk factors.
“Despite some recent evidence suggesting adverse cardiovascular effects of habitual vigorous exercise, our findings show no sign of a plateau effect with elite fitness,” Dr. Jaber notes. “These results underscore the importance of aerobic fitness to overall health, which rivals that of traditional risk factors.”
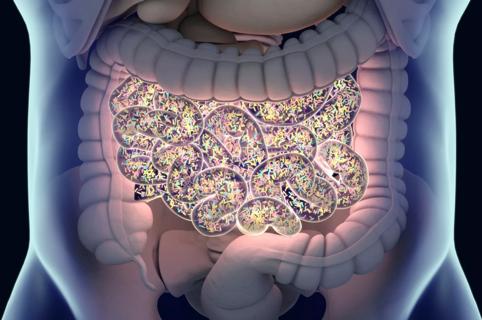
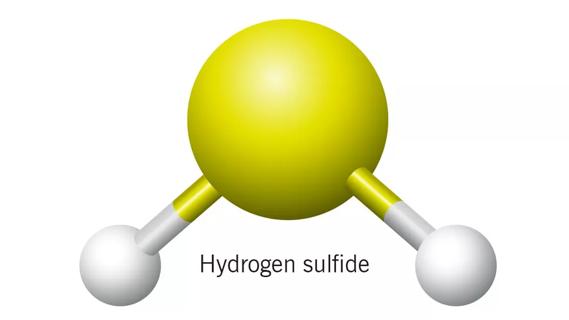
A new drug class promises a novel approach to reducing platelet hyperresponsiveness and thrombosis potential without increased bleeding risk by nonlethally targeting the gut microbial pathway that produces the atherogenic metabolite TMAO. The drug class — known as known as halomethylcholines, or mechanism-based inhibitors — was developed by Cleveland Clinic researchers and tested in a mouse model of arterial injury. “Outside of antibiotics, which cannot be used chronically without generating resistance, this is the most potent therapy to date for ‘drugging’ the microbiome to alter a disease process,” says lead researcher Stanley Hazen, MD, PhD.
A single oral dose of a halomethylcholine significantly reduced plasma TMAO levels in the mouse model for up to three days and reversed enhanced platelet responsiveness and thrombus formation following arterial injury — without taking platelet function below normal. The agents were minimally absorbed into the body and remained in the gut, where they selectively accumulated in gut microbes. Because these compounds were designed not to kill bacteria, they are not expected to induce antibiotic resistance.
“We showed that gut bacteria were altered but not killed by these therapies, with no observable toxic side effects,” Dr. Hazen says. “This approach could potentially be used to target other gut microbial pathways while minimizing systemic drug exposure and antibiotic resistance. We’ve identified a new potential target for treating individuals at risk for thrombotic complications and cardiovascular disease.”
(J Am Coll Cardiol. 2018;72:650-659)
Patients’ baseline risk factors for mortality at the time of listing for heart transplantation quickly become nonsignificant once subsequent events and changes in lab values reflecting organ failure are incorporated into a dynamic model that continuously updates mortality risk. So found a unique study of 414 patients listed for heart transplant at Cleveland Clinic from 2008 to 2013. The study sought to develop a decision aid to aggregate adverse events and metrics of end-organ function into a continuously updated estimate of waitlist mortality.
Of the 414 patients, 77 died while on the waitlist, yielding one- and four-year survival rates of 85 and 57 percent, respectively. The pre-listing patient factors used in existing heart failure survival models were not predictive of survival when time-varying factors were taken into account while patients were on the waitlist. Neurological events, new requirement for dialysis, respiratory complications and increased serum bilirubin and creatinine were the time-varying factors most predictive of waitlist mortality.
The Cleveland Clinic researchers are now building on these insights in an NIH-funded collaboration with four other U.S. centers (detailed here) to develop the first tool to dynamically update heart transplant waitlist mortality risk using variables not included in existing models as well as serial clinical assessments. “A continuously updated mortality estimate, combined with clinical evaluation, may inform patient status changes that could reduce mortality on the heart transplant waitlist,” concludes lead researcher Eugene Blackstone, MD.
(JACC Cardiovasc Interv. 2018;11:2207-2216)
The randomized PARTNER 2A trial comparing surgical (SAVR) with transcatheter (TAVR) aortic valve replacement in patients with severe aortic stenosis at intermediate surgical risk keeps yielding useful insights through its many subanalyses. This latest one took on a previously unexplored question: Whether prior cardiac surgery confers increased risk for adverse clinical outcomes in intermediate-risk patients undergoing TAVR as it has been shown to do in those undergoing SAVR.
Of the 2,032 patients in PARTNER 2A, 509 (25 percent) had prior cardiac surgery, mostly coronary artery bypass grafting. When patients were stratified by whether or not they had prior cardiac surgery, short- and long-term clinical outcomes (all-cause death and disabling stroke) over two years were statistically comparable between the TAVR and SAVR groups regardless of whether patients did or did not have prior cardiac surgery. However, major vascular complications and life-threatening bleeds at 30 days were disproportionately more common among patients with prior cardiac surgery who underwent SAVR.
“This subanalysis supports the long-term efficacy of both TAVR and SAVR in intermediate-risk patients who have had prior cardiac surgery, although there may be a possible early safety advantage with TAVR in this group,” says PARTNER 2A co-investigator Lars Svensson, MD, PhD, Chair of Cleveland Clinic’s Heart & Vascular Institute. “These findings underscore the importance of caring for this subpopulation with a comprehensive heart valve team approach that can adjust for nuances in patient preferences and vascular characteristics.”
(N Engl J Med. 2018;379:1007-1016)
When the multicenter phase 3 ATTR-ACT study was published a few months ago, it provided the first-ever evidence of therapeutic benefit against the ATTR form of cardiac amyloidosis outside of heart transplantation. Among 441 patients with the condition, the small-molecule compound tafamidis was associated with significantly lower rates of all-cause mortality at 30 months relative to placebo (30 percent vs. 43 percent) as well as significantly fewer cardiovascular-related hospitalizations. Adverse events in the tafamidis and placebo arms were comparable.
“The degree of survival benefit from tafamidis was impressive,” says Cleveland Clinic cardiologist Mazen Hanna, MD, lead investigator of the ATTR-ACT trial at Cleveland Clinic and a co-author of the published study. “It will change the landscape of this disease and offers long-awaited hope to our patients with wild-type TTR cardiac amyloidosis in addition to those with the hereditary variant.” FDA approval of tafamidis is expected in 2019.
Dr. Hanna also sees tafamidis playing a key role in future combination regimens against ATTR amyloidosis, along with other emerging therapies. “This period reminds me of the time when effective HIV therapies first emerged,” he says. “We believe the future will be combination therapy, with the goal of soon turning amyloidosis into a chronic disease patients can live with for a long time.”
(J Thorac Cardiovasc Surg. 2018;156:750-759)
Risk stratification for sudden cardiac death (SCD) in patients with obstructive hypertrophic cardiomyopathy (HCM) needs some refining, especially for patients who undergo myectomy. So concluded a retrospective observational study of 1,809 consecutive patients with obstructive HCM evaluated at Cleveland Clinic. The study found little correlation between actual rates of SCD and the rates predicted by SCD risk models in recent guidelines from the European Society of Cardiology (ESC) or the American College of Cardiology/American Heart Association (ACC/AHA). “For example, in the highest SCD risk group, the actual five-year event rate was only about half the expected rate based on ESC risk score,” observes co-author Nicholas Smedira, MD, a Cleveland Clinic cardiac surgeon.
A full 64 percent of patients underwent surgical myectomy to relieve their obstructive HCM. Multivariable analysis showed that myectomy — and, separately, atrial fibrillation during follow-up — was associated with significantly reduced risk of longer-term SCD, whereas ESC and ACC/AHA risk scores were not. The researchers concluded that adding myectomy and atrial fibrillation to the ESC and ACC/AHA risk scores for SCD significantly reclassified risk and provided incremental prognostic utility.
“Our study suggests that relieving the obstruction in HCM, debulking the thick myocardium, can potentially have an impact in reducing sudden death,” says Cleveland Clinic cardiologist and lead author Milind Desai, MD. “I think we’re entering an era with surgical myectomy where we’re talking not just about symptom relief but also about modulating longer-term risk of dying.”
(Circulation. 2018;138:1749-1751)
Women with mitral valve disease undergo mitral valve replacement at higher rates than their male counterparts do, and this has been linked to persistently poorer mitral valve surgery outcomes in women. Despite this linkage, studies to date have generally not accounted for sex differences in the etiology of surgical mitral valve disease or any changes in etiology over time. To fill that gap, researchers from Cleveland Clinic analyzed 23,806 consecutive patients who underwent primary mitral valve replacement or repair at the institution from 1993 to 2016.
The analysis revealed highly significant (P < .001) between-sex differences in prevalence of the three main types of mitral valve disease — degenerative, ischemic and rheumatic — in the cohort, with much higher rates of rheumatic disease in women and much higher rates of degenerative disease in men. Despite changes in the prevalence of each etiology over the study period (degenerative disease became more common, and rheumatic and ischemic disease grew less common), the between-sex differences in each of the disease types remained consistently significant throughout the study.
“Our analysis clarifies that, despite a temporal shift in etiology of surgically treated mitral valve disease overall, differences between the sexes persist into the modern era of cardiac surgery,” notes co-author Leslie Cho, MD, Director of Cleveland Clinic’s Women’s Cardiovascular Center. “We’ve identified another potential explanation for sex differences in procedure selection and outcomes.”
Large-scale joint study links elevated TMAO blood levels and chronic kidney disease risk over time

Investigators are developing a deep learning model to predict health outcomes in ICUs.
International collaboration is most genetically diverse study of the disease to date

Preclinical work promises large-scale data with minimal bias to inform development of clinical tests
Cleveland Clinic researchers pursue answers on basic science and clinical fronts

Study suggests sex-specific pathways show potential for sex-specific therapeutic approaches

Cleveland Clinic launches Quantum Innovation Catalyzer Program to help start-up companies access advanced research technology

Research project aims to pinpoint biomarkers that could speed diagnosis