Cleveland Clinic researchers pursue answers on basic science and clinical fronts
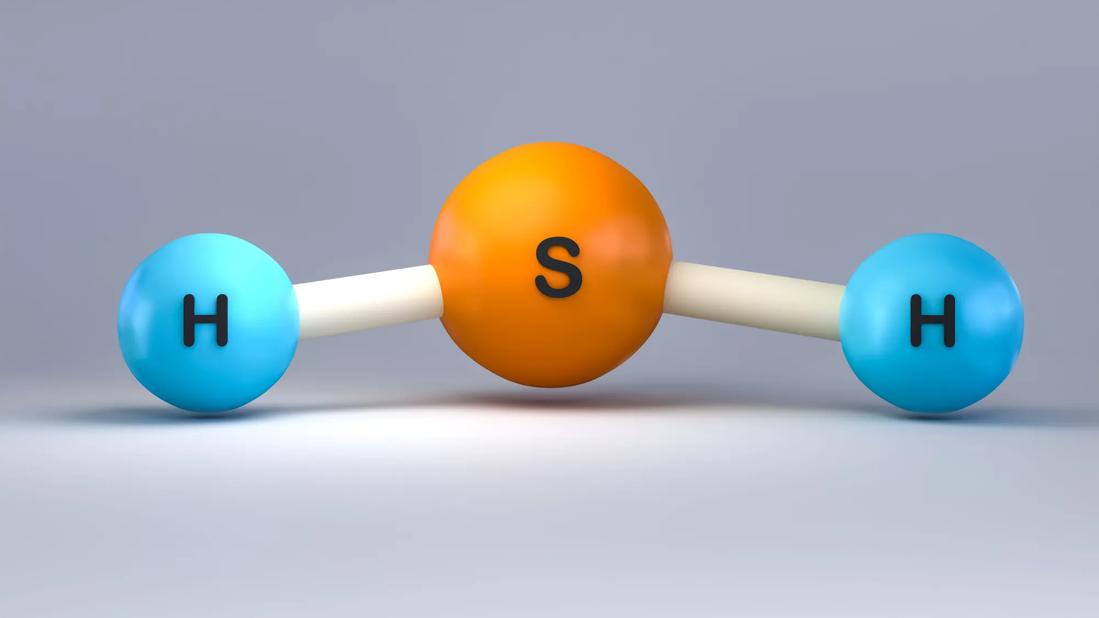
New Cleveland Clinic research efforts are exploring the cancer-suppressing effects of endogenous hydrogen sulfide (H2S) in glioblastoma and whether aging-induced decreases in H2S can be effectively targeted therapeutically.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The efforts are being pursued via basic science investigations led by Christopher Hine, PhD, with support from a $2.5 million, five-year grant from the National Institute of Neurological Disorders and Stroke (NINDS), as well as in a proof-of-concept clinical trial led by medical oncologist David Peereboom, MD.
“We believe this research is important and promising enough to pursue on the two fronts simultaneously,” says Dr. Hine, assistant staff in the Department of Cardiovascular and Metabolic Sciences in Cleveland Clinic Lerner Research Institute.
The backdrop for this work is the recognition of two key facts about H2S, a byproduct of cysteine metabolism. First, H2S inhibits the growth of glioblastoma cells in culture and mitigates the in vivo progression of glioblastoma tumors. Additionally, the body’s production of H2S decreases as humans age. Previous preclinical investigations by Dr. Hine and colleagues made important contributions to these insights.
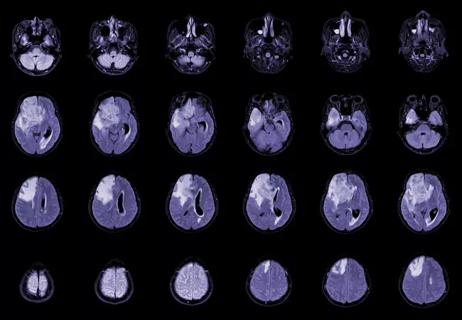
In one study (J Clin Invest. 2021;131[17]:e138276), Dr. Hine’s lab and that of his Lerner Research Institute colleague Justin Lathia, PhD, demonstrated that diet-modifiable H2S signaling suppresses glioblastoma by restricting metabolic fitness, while loss of H2S signaling spurs cancer stem cell enrichment and disease acceleration.
“We found that H2S acts as a tumor suppressor against glioblastoma,” Dr. Hine explains. This insight, together with evidence that endogenous H2S production and signaling are reduced in human glioblastoma brain tissue relative to noncancerous brain tissue, prompted interest in boosting H2S levels as a therapeutic strategy. “These findings suggested that interventions that increase H2S bioavailability might be used with standard-of-care glioblastoma therapy to improve outcomes for patients.”
Advertisement
Because clinical use of exogenous H2S is limited by toxicity and volatility, the group’s interest focused on bolstering endogenous H2S synthesis. Previous work by Dr. Hine had shown that thyroid hormone signaling suppresses H2S production (Cell Metab. 2017;25[6]:1320-1333.e5). “That led us to hypothesize that lowering thyroid hormone signaling might reduce that suppression and thus boost endogenous H2S, thereby promoting glioblastoma tumor suppression,” he observes.
This hypothesis was further bolstered by published data describing the use of the thyroid hormone inhibitor propylthiouracil (PTU) to promote endogenous H2S production in mice, as well as by a small 2003 clinical trial at Cleveland Clinic (Anticancer Res. 2003;23[1B]:617-626) in which oral PTU was found to prolong survival in patients with high-grade glioma treated with high-dose tamoxifen. “That study showed that making patients hypothyroid could extend survival threefold compared with patients who didn’t have their thyroid hormone signaling reduced,” Dr. Hine notes.
In the 20 years since that small clinical study, PTU has largely been supplanted in clinical endocrinology by oral methimazole, a safer and more efficient thyroid hormone inhibitor. “The availability of a more clinically favorable option for thyroid hormone inhibition gave us reason to resurrect the therapeutic approach from that prior Cleveland Clinic trial, albeit with a different mechanism in mind,” Dr. Hine explains.
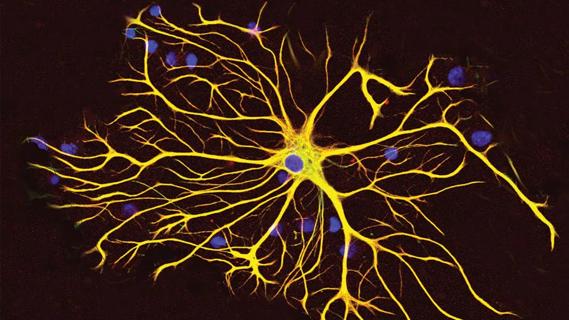
Within this context, Dr. Hine and co-investigator Dr. Lathia are using their NINDS grant to investigate the tumor microenvironment in a murine model of glioblastoma. They are comparing standard mice with mice lacking an enzyme key to H2S production and with others that overexpress the enzyme. “The hypothesis is that, following glioblastoma cell implantation, tumor growth will be much faster in the mice that lack the enzyme and much slower in those that overexpress the enzyme,” Dr. Hine says.
Advertisement
The researchers are also examining host-tumor interactions on the level of H2S and thyroid hormone to determine whether changes in H2S production derive from the glioblastoma cells themselves or from noncancerous tissue — or whether their origins may be systemic in nature. “We’re exploring whether it’s basically a host response or a tumor-specific response to the H2S,” Dr. Hine says.
Additionally, the researchers will administer the thyroid hormone inhibitors PTU and methimazole to the mice to confirm whether and how much these drugs’ antithyroid-related promotion of H2S production suppresses the tumors.
Meanwhile, Dr. Hine’s clinical colleague David Peereboom, MD, is leading a small phase 2 clinical trial to evaluate the safety and effects of using methimazole to suppress thyroid hormone signaling in patients with progressive glioblastoma. The open-label trial will enroll up to 19 patients undergoing surgical resection for recurrent glioblastoma. Patients will receive daily oral methimazole for at least five days preoperatively, to lower circulating thyroid hormone levels, and then for four weeks postoperatively. Secondary chemotherapy will then be added at the treating physician’s discretion.
“We hypothesize that reduced thyroid hormone production via treatment with methimazole will bolster the effectiveness of therapy for glioblastoma and extend survival by boosting H2S production and function within the tumor-bearing brain,” Dr. Peereboom observes. “The goal is to provide proof of concept that suppression of thyroid hormone signaling with methimazole and subsequent augmentation of H2S synthesis and signaling is safe and feasible in patients with glioblastoma.”
Advertisement
While positive results from the clinical trial would guide further development of the clinical investigators’ combinatorial therapeutic approach, Dr. Hine is likewise anticipating next research steps from a basic science standpoint. Key questions include whether H2S exerts its antitumor effects in glioblastoma by modifying the immune system and whether there are other means of enhancing H2S signaling in patients apart from treatment with thyroid hormone inhibitors.
“The clinical study of methimazole in this setting is exciting, but there may ultimately be a more direct means of boosting H2S in these patients without inducing a hypothyroid state,” Dr. Hine concludes.
Advertisement
Advertisement

Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies

Advances in genomics, spinal fluid analysis, wearable-based patient monitoring and more

Researchers use AI tools to compare clinical events with continuous patient monitoring

Combining dual inhibition with anti-PD1 therapy yielded >60% rate of complete tumor regression
New research from Cleveland Clinic helps explain why these tumors are so refractory to treatment, and suggests new therapeutic avenues

Presurgical planning and careful consideration of pathology are key to achieving benefits
Study demonstrates its role in tumor lethality, raises prospect of therapeutic targets

Focused ultrasound is paired with ALA to utilize sonodynamic therapy to target cancer cells