Custom components offer better outcomes when conventional options fail
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Revision arthroplasty of severe acetabular defects has entered a new era thanks to additive manufacturing (3D printing) of custom implantable components.
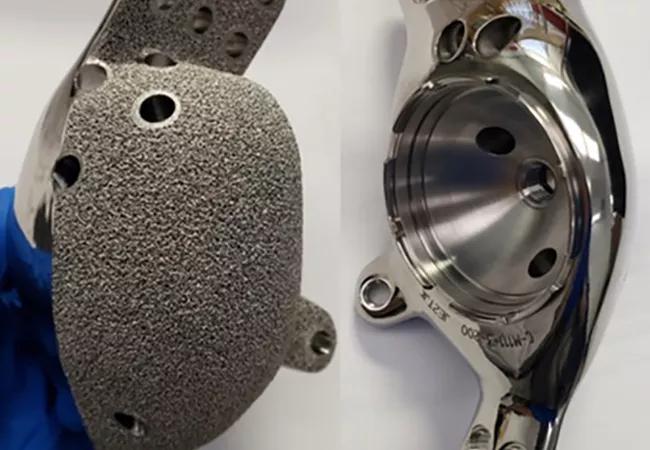
For more than two decades, we in Cleveland Clinic’s Department of Orthopaedic Surgery have worked with implant manufacturers to custom design components milled out of titanium. However, most recently we have collaborated with Stryker Corporation to establish a 3D-manufacturing program that produces customized titanium components with a porous surface, similar to cancellous bone, to facilitate bony ingrowth.
This technology has helped improve outcomes for patients with severe hip defects that cannot be repaired through conventional methods — or even with other custom implants.
For example, one patient came to Cleveland Clinic after having multiple failed hip replacements. She presented with a loose implant and a pelvis full of metal debris (Figure 1). We removed the loose implant and inserted a temporary hip and a bone graft while we explored long-term treatment options. Because the patient’s hip had a huge defect, with no proximal femur and no pelvis, permanent reconstruction was not possible with existing implants and standard technology.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b749a26d-e8b5-42b0-9a8b-4a641b5b8559/22-ORI-3225208-CQD-Inset1_jpg)
Figure 1. X-ray showing a loose implant in a patient with multiple failed hip replacements.
We submitted CT scans of the patient’s hip to the implant manufacturer, who used them to render a 3D model. We then began an iterative design process (Figure 2). The surgical and manufacturing teams held virtual meetings to discuss shapes to fit the model. Next, the teams worked together to determine the placement of porous surfaces. This was based on careful evaluation of the detailed CT scan and virtual pelvic model that could be manipulated in real time. By identifying the most robust and healthy remaining pelvic bone, we were able to create surfaces on the custom implant to interface with the patient. These bioactive porous surfaces were designed to allow ingrowth of host bone into the custom component.
Advertisement
The actual design process for these 3D-printed titanium implants is eight to 12 weeks. At this time, the longest and most tedious portion of the design is the regulatory process and compassionate release of the implants through the Food and Drug Administration (FDA) and Cleveland Clinic’s Institutional Review Board. This is necessary to assure safety and appropriate use of this type of implant. The actual print time for the implant is approximately four to five days, then it requires further processing and machining before it can become a final implant that is shipped and ready for implantation.
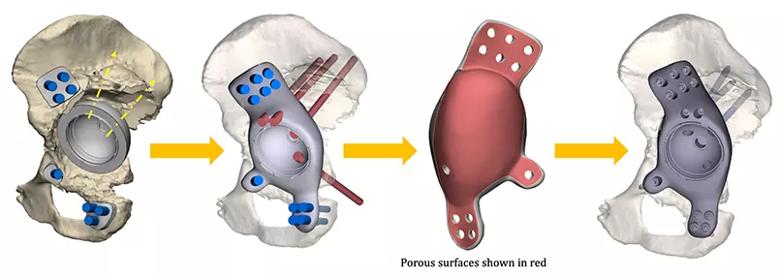
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/97048d30-6007-43f5-aa37-fddefcdbf906/22-ORI-3225208-CQD-Inset2_jpg)
Figure 2. The iterative design process, from concept to implant. Graphics courtesy of Stryker Corporation.
For the patient in this case, the result was a custom 3D-printed pelvis (Figures 3-5).
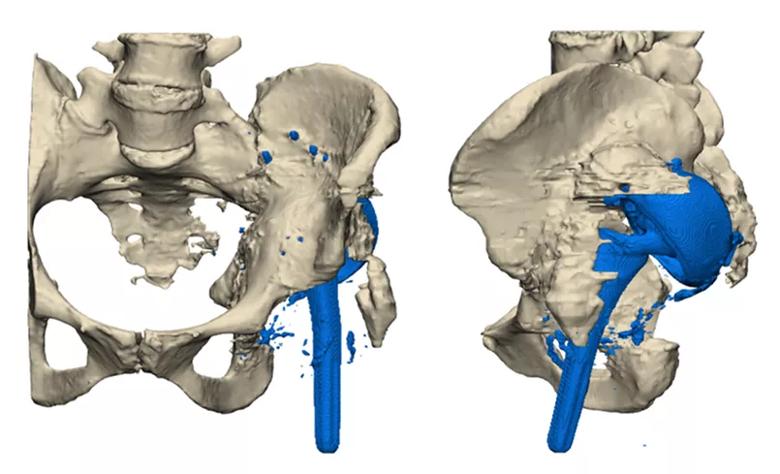
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f7f318cd-c068-4b49-8c7b-1ea97adc3f35/22-ORI-3225208-CQD-Inset3_jpg)
Figure 3. The patient’s initial condition and placement of original implants.
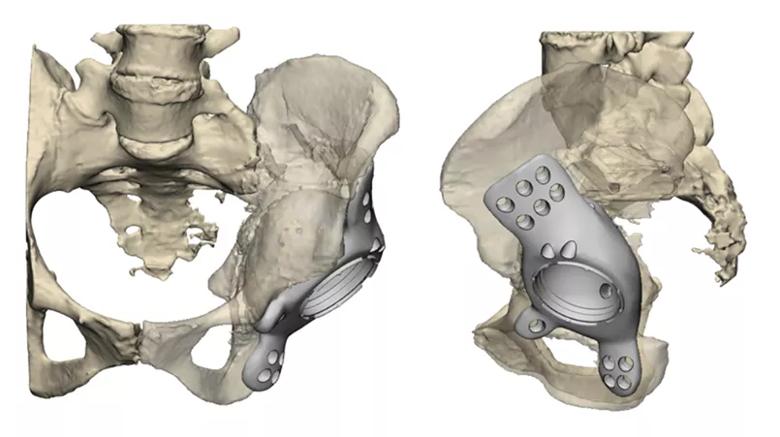
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b804ccb3-a56a-4747-badd-1ee4c47c4ddc/22-ORI-3225208-CQD-Inset4_jpg)
Figure 4. Final implant plan developed by the surgical and manufacturing teams.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/6029d856-178b-4680-aa15-5181a5e20108/22-ORI-3225208-CQD-Inset5_jpg)
Figure 5. Final manufactured implant.
The surgery is a major revision hip procedure and requires extensile exposure and detailed knowledge of pelvic anatomy. These procedures can last from five to eight hours and are a significant stress on the patient. Because of the close proximity to major neurovascular structures during the entire procedure, the surgical techniques are cautious and precise to avoid complications. We also use evoked nerve monitoring to help protect the sciatic nerve, which is often in the surgical field.
Now two years after surgery, the patient is walking without pain (Figure 6).

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/bbbb75b5-67a7-49ce-8521-88e655b212a7/22-ORI-3225208-CQD-Inset6-631x1024_jpg)
Figure 6. Final placement of the 3D-printed implant.
Since 2020, we have designed and implanted custom 3D-printed acetabular prosthetics for multiple patients, including those with no anatomy to support conventional implants and no ability to walk.
Alternative custom implants are available. However, most have a gritted titanium surface rather than a porous surface and, therefore, often fail to biologically integrate into the patient’s bone, causing a higher risk of loosening. We have not observed these issues with 3D-printed porous surfaces in the short term, and we believe that they will have the opportunity to provide lasting biologic fixation and better long-term outcomes.
Advertisement
Technology for 3D-printing joint implants has become widely used in Europe over the last five years. Now the FDA grants expanded access for compassionate use in the U.S. From diagnosis to Institutional Review Board approval, FDA approval, design, manufacturing and surgery, the process currently takes about three months.
Cleveland Clinic is one of few centers in the U.S. to offer this novel service and has among the highest patient volumes. Using custom 3D-printed components has become standard at Cleveland Clinic for the treatment of failed joint replacements when conventional reconstructive options are not possible.
Dr. Krebs is Vice Chairman in Cleveland Clinic’s Department of Orthopaedic Surgery, and Director of Cleveland Clinic’s adult reconstruction fellowship program. His specialty interests include complex adult reconstructive surgery, robotics and total joint replacement. Dr. Krebs is a paid consultant for Stryker Corporation and receives royalty payments for implants and inventions commercialized through the company.
Advertisement
Advertisement

How it’s similar but different from the direct anterior approach

Should surgeons forgo posterior and lateral approaches?

Multidisciplinary care can make arthroplasty a safe option even for patients with low ejection fraction

High-risk procedure prepares patient for lifesaving heart surgery

Cleveland Clinic is among the first in the U.S. to perform the procedure

Insights to help orthopaedic practices comply with the 2025 CMS mandate

Dr. Piuzzi wins 2025 Kappa Delta Young Investigator Award for pioneering work

For patients with anatomic abnormalities, substantial bone loss and pre-existing hardware