Offers adequate exposure of normal and abnormal anatomy
After ignoring the pain in his hip for several years, a 68-year-old man decided to pursue total hip arthroplasty (THA). Unfortunately, his decision coincided with the COVID-19 pandemic, and he was forced to delay surgery. When the patient finally presented two years later, his osteoarthritis was severe. His hip joint had deteriorated so much that it had collapsed and healed, the ball fusing into the socket.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/74714f7e-c0bc-4418-b2d6-a44d6817451e/23-ORI-3641509-CQD-Inset1_jpg)
Preoperative standing anteroposterior radiograph showing severe left hip arthritis with ankylosis of the hip.
“His biggest complaint was the pain and stiffness,” says orthopaedic surgeon Matthew Deren, MD. “His gait was awkward because he couldn’t move his hip at all. He couldn’t even sit in a chair normally. His leg also was shorter on the affected side due to pelvic obliquity.”
Although more than 450,000 THAs are performed in the U.S. annually, it’s “pretty rare” to see an auto-fused hip, says Dr. Deren. “They’re generally a difficult surgery because you can’t move the hip at all to position it or get into the joint. It’s a lot more challenging, it takes longer, and there can be a lot of complications.”
Patients with fused (ankylosed) hips aren’t always eligible for surgery due to the complexity, but as long as hip abductor muscles are functional, outcomes of THA in auto-fused hips can be good, Dr. Deren says. For the patient in this case, THA was recommended because the hip muscles were intact and functioning before the hip became fused.
While the anterior approach for THA is becoming more common, many surgeons feel that it will not give them sufficient exposure for complex cases. Dr. Deren, however, prefers to perform most THAs anteriorly, including surgeries for ankylosed hips.
“When the body fuses a hip, it externally rotates and flexes it, putting the hip in perfect position for the anterior approach,” he says. “With a posterior approach, it would be difficult to get into the hip because everything is fairly closed and contracted on the other side. With the anterior approach, the hip is wide open and accessible.”
Advertisement
Dr. Deren uses intraoperative fluoroscopy to see exactly where a socket should be recreated in the flat wall of pelvic bone.
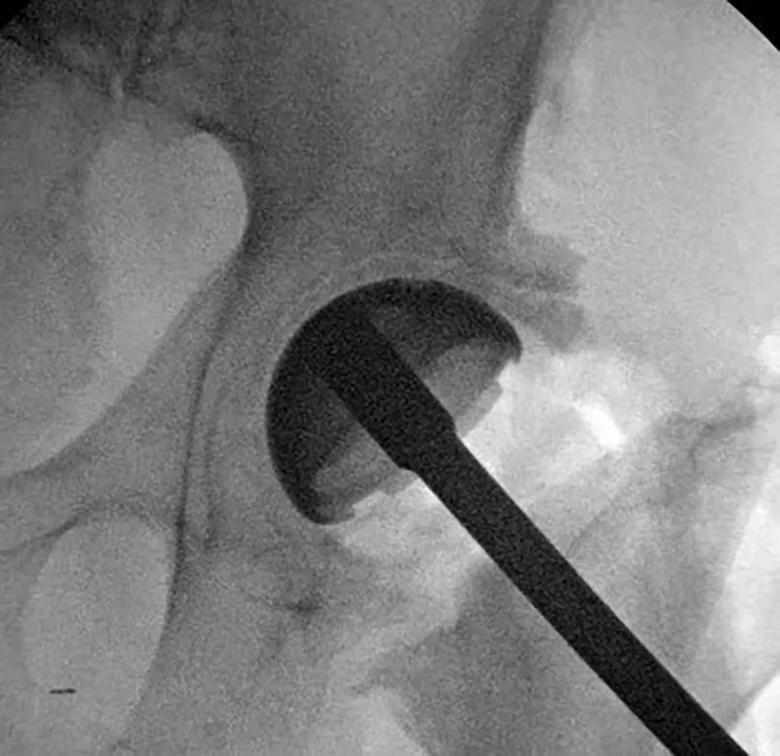
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/857fab7a-667a-4051-8204-2b9e617994ee/23-ORI-3641509-CQD-Inset2_jpg)
Intraoperative fluoroscopy view showing position of the acetabular component upon insertion after reaming a new socket.
The combination of anterior approach and intraoperative fluoroscopy causes the procedure to take slightly longer than a conventional THA.
“Most surgeons think of this as a more complex surgery that they wouldn’t do anteriorly, but an anterior approach allows adequate exposure of all the anatomy — normal and abnormal — so you can perform the surgery as directly as possible,” says Dr. Deren.
After the procedure, the patient spent two days in the hospital, slightly longer than patients having conventional THA. His pain was minimal. Now two months later, the patient continues to manage pain well. His pelvic obliquity has been improved.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/35d84ba4-9eda-407a-bdb1-f0e6035e5619/23-ORI-3641509-CQD-Inset3_jpg)
Postoperative radiograph demonstrating well-placed components and improvement in pelvic obliquity from takedown of the ankylosed hip.
“The patient’s biggest challenge has been regaining motion,” says Dr. Deren. “That is not unexpected because he hadn’t been able to move normally for a few years before surgery. All those muscles and ligaments need to stretch. With more physical therapy, I’m confident that he will be able to sit normally and continue to walk normally.”
Advertisement
Advertisement
How it’s similar but different from the direct anterior approach
Should surgeons forgo posterior and lateral approaches?
Multidisciplinary care can make arthroplasty a safe option even for patients with low ejection fraction
High-risk procedure prepares patient for lifesaving heart surgery
Cleveland Clinic is among the first in the U.S. to perform the procedure
Insights to help orthopaedic practices comply with the 2025 CMS mandate
Dr. Piuzzi wins 2025 Kappa Delta Young Investigator Award for pioneering work
For patients with anatomic abnormalities, substantial bone loss and pre-existing hardware