Cleveland Clinic study finds it’s safe and effective
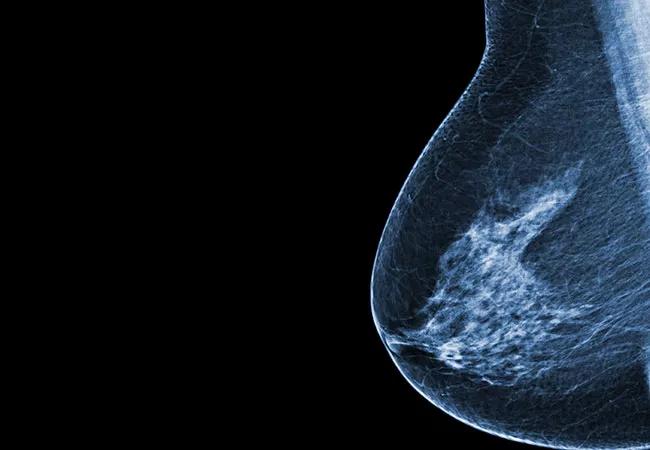
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3c46a9ef-b31d-426d-bb01-5176a15b44c8/650x450-Breast-Cancer_jpg)
650×450-Breast-Cancer
Lymphatic mapping is essential to performing sentinel lymph node biopsy (SLNB) and staging for early-stage breast cancer. Standard mapping techniques — colloid radiotracer labeled with technetium 99 (99mTc) or visible blue dye (methylene blue or isosulfan blue) — are highly accurate, especially when used in combination, with a detection rate of approximately 99%.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
However, they have significant drawbacks. 99mTc requires nuclear licensing as well as preparing, handling and disposing of nuclear material. It also involves a painful injection, which is usually administered by a radiologist before surgery. Blue-dye injections can be administered during surgery, but they may cause skin necrosis and anaphylaxis and have only a 91% detection rate when used alone.
Indocyanine green (ICG) is a fluorescent dye that can be detected using a near infrared (NIR) camera. It has been used for more than 50 years and has an excellent safety profile. It is currently used for image-guided procedures, such as NIR angiography of blood vessels and skin flap perfusion for mastectomies.
ICG with NIR imaging is the standard technique for lymphatic mapping in Japan (which conducted the first ICG trials) and Europe.
ICG has many potential advantages over other lymphatic mapping techniques. It can be administered during surgery, provides instant visualization with NIR, and is less costly since it requires no special handling.
Recent studies from Japan and Europe have found that 99mTc and ICG have comparable lymph node detection rates. Cleveland Clinic conducted the first U.S. study to prospectively compare ICG to 99mTc for breast cancer axillary SLN lymphatic mapping.
“We are always looking for better solutions,” says Stephen Grobmyer, MD, Director of the Breast Center and Co-leader of the Comprehensive Breast Cancer Program at Cleveland Clinic. “I saw how well ICG worked for breast cancer lymph node mapping in Japan. With fluorescent imaging becoming more widely used, it was an option we wanted to investigate.”
Advertisement
From 2016 to 2018, Cleveland Clinic’s study enrolled 92 female patients (median age 59) with stage T1 or T2 clinically node-negative breast cancer undergoing either a lumpectomy or mastectomy.
All participants underwent lymphatic mapping with both 99mTc and ICG. 99mTc was performed preoperatively and ICG at the time of operation while the patient was under anesthesia.
One patient had failed SLN mapping with both techniques, which left 91 patients for SLN analysis.
A total of 235 SLNs containing one or both of the tracers were identified. The median number of SLNs removed with ICG was 2 (range 1 to 7), the same median number removed with 99mTc (range 0 to 5).
Dual tracer was found in 191 (81%) SLNs. ICG alone identified 33 (14%) additional SLNs, and 99mTc alone was found in 11 (5%) SLNs. The two-sided 95% CI for the difference in proportions of SLNs detected by the two methods was 0.036 to 0.151, which shows that ICG SLN mapping is equivalent to 99mTc in SLN identification.
Pathologically positive axillary SLNs were found in 18 of 91 patients (19.7%). Among these patients, there were 24 positive SLNs — 10.2% of all 235 SLNs removed. ICG identified 24 of 24 (100%) positive SLNs and 99mTc identified 23 of 24 (96%) positive SLNs.
The median lymphatic transit time from ICG injection to the start of SLN excision was just five minutes, another advantage of this technique. Patients with a higher BMI had a longer transit time, but all SLNs were able to be identified.
Based on this study’s results, “ICG is a safe and efficacious technique that should be considered an option for breast cancer lymph node mapping,” says Dr. Grobmyer.
Advertisement
Cleveland Clinic’s Division of Breast Services is working on further developing ICG NIR imaging with tools such as wearable fluorescent glasses. They are also exploring other uses for this technology, such as evaluating lymphatic flow and repairing lymphatic leaks.
“ICG NIR imaging has the potential to make surgery safer, faster and more accurate, especially as the imaging technology and dyes become more sophisticated,” says Dr. Grobmyer.
Advertisement
Advertisement
Goal-of-care discussions drive earlier hospice access
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting