ASTRO 2017 abstract finds radiosensitivity variants
While molecular tumor profiling and genomic medicine have opened new vistas in personalized cancer treatment and small-molecule drug discovery, the impact of many genomic variants on radiosensitivity remains largely unknown.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A new pan-cancer inventory of genomics data, developed by Mohamed Abazeed, MD, PhD, and Brian Yard, PhD, aims to bring some clarity to what many radiation oncologists have long suspected — that clinically relevant variants in personalized drug therapy have some bearing on tumor response to radiation.
“In the era of precision medicine, clinically actionable alterations for the radiation oncologist have lagged behind compared to the substantial progress made in the use of targeted drug therapies,” says Dr. Yard, a research fellow at Cleveland Clinic Cancer Center. “In this study, we seek to annotate an inventory of genetic variants that regulate radiosensitivity.” Dr. Yard will present results at ASTRO 2017.
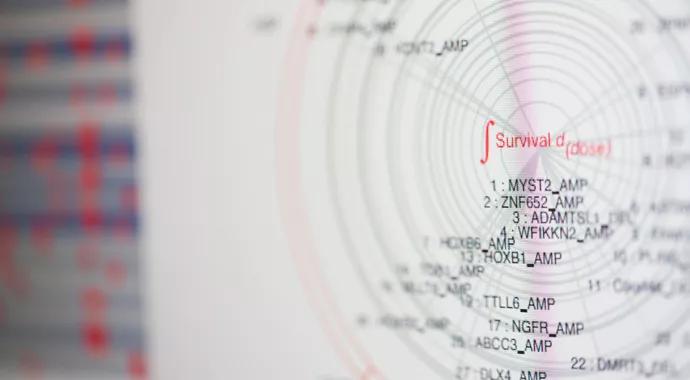
The study initially compiled genomic variants using previously published results that measured response to radiation across more than 500 cancer cell lines from the Broad Institute’s Cancel Cell Line Encyclopedia (CCLE). The investigators then systemically interrogated variants using a new profiling platform that measures the activity of individual variants in isolation, removing confounding influences of other tumor-associated variants.
Results show that variants correlated with radiosensitivity tend to have four common characteristics: close association with DNA damage response, G1/S cell cycle transition regulation, intrinsic apoptotic systems and cell growth signaling.
With these core components identified, Drs. Yard and Abazeed compiled a list of radioresistant variants that could become the first draft of a treatment planning aid for precision radiotherapy.
Advertisement
Armed with that exploratory layer of data, the team then prioritized further investigation of more than 200 open-reading frames (the portions of codons that code for amino acids, rather than control mechanisms) based on three variables: cell-line association with radiation resistance, location within conserved protein domains (UniProt) and predicted functional impact (MutationAssessor).
Site-directed mutagenesis generated the mutant clones and transferred the ORFs into lentiviral vectors for stable expression in immortalized bronchial and mammary gland cell lines.
A high-throughput platform developed by Drs. Yard and Abazeed measured survival in the immortalized cell lines. This ultimately led to a lab-based assessment of the effect of individual variants on response to radiation.
“We have been working toward this for many years,” says Dr. Yard. “For the first time, we have adapted our high-throughput profiling platform to assess radiosensitivity of individual variants expressed in immortalized cell lines.”
The ASTRO abstract and planned publication represents a culmination of several years of work in developing methodologies and statistical analyses that could forecast tumor response to radiotherapy. With ASTRO underway and the data soon to be published in full, Drs. Abazeed and Yard have plans to take their work into the clinic.
“We are elucidating new biological mechanisms that are helping us unravel the complex interactions between radiation and the tumor,” says Dr. Abazeed, associate staff in the departments of Radiation Oncology and Translational Hematology and Oncology Research. “The natural extension of this work is to incorporate this information capability into predictive models for radiation planning.” The ultimate arbiter of success of this work, he continues, is improved outcomes for patients receiving radiotherapy.
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient