20 months later, IOP remains well controlled
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 29-year-old male was referred to the glaucoma service at the Cole Eye Institute for significant optic disc cupping with an IOP around 12 mm Hg in each eye. His ocular history was significant only for prior strabismus surgery. On initial examination, his vision was 20/20 OU with a low myopic correction. IOP OD remained 12, but the left eye had increased to 40 in the six weeks since he was seen by the referring ophthalmologist. Anterior segment exam was normal OD. The left eye had a few anterior chamber cells and atrophy of the nasal iris sphincter. Gonioscopy was unremarkable OU.
Fundus exam OD revealed a large disc with no focal rim thinning and a cup-to-disc ratio (CD) of 0.8. CD ratio OS was 0.95 with severe diffuse rim thinning. The left eye also had a previously undetected large area of retinal atrophy with subretinal and intraretinal fluid encompassing most of the superonasal quadrant and extending posteriorly to the optic disc. Visual fields demonstrated an inferotemporal arcuate defect OS consistent with retinal findings, and optical coherence tomography showed a diffusely thinned retinal nerve fiber layer OS greater than OD. The extracted optic disc tomograms OS demonstrated subretinal fluid in the superonasal peripapillary region. Further questioning revealed that three years prior, this young man’s left eye had been hit with a tennis ball.
While the low grade anterior chamber cell with fluctuation and markedly elevated IOP suggested an inflammatory glaucoma like Posner-Schlossman, herpetic iridocyclitis or sarcoid uveitis, the retinal detachment led us to include Schwartz-Matsuo syndrome in the differential diagnosis. This patient was prescribed dorzolamide-timolol and prednisolone acetate 1%, each b.i.d. OS, and referred to the retina service for their opinion and expertise.
Advertisement
Three days later, his IOP had improved to 16, and Schwartz-Matsuo syndrome was confirmed when the retina service diagnosed a chronic combined schisis/detachment with a traumatic retinal dialysis. Surgical repair would be technically challenging due to his attached hyaloid, phakic status, prior strabismus surgery complicating buckle placement, and giant retinal tear. Therefore, given his well-controlled IOP, the patient was observed initially by both the glaucoma and retina services. Eventually, however, his retinal detachment progressed inferiorly toward the macula, and surgical repair was accomplished via combined pars plana vitrectomy and scleral buckle.
Although the retinal reattachment surgery was successful, his IOP quickly became uncontrolled postoperatively, reaching 29 mm Hg on four topical glaucoma medications and acetazolamide 1000 mg daily.
Schwartz-Matsuo is a rare type of glaucoma. In this condition, a chronically detached retina sheds photoreceptor outer segments, which in turn clog trabecular meshwork outflow, increase outflow resistance and lead to a secondary open-angle open glaucoma. The cells seen in this patient’s anterior chamber were not inflammatory cells, but rather actual photoreceptor segments circulating in the aqueous fluid. As would be expected, these cells are not responsive to topical corticosteroids.
While I typically address intractable glaucoma after vitreoretinal surgery with a tube implant, that surgery wasn’t ideal in this situation. This patient’s scleral buckle and prior strabismus surgery would complicate glaucoma drainage device implantation. Furthermore, implantation of a glaucoma drainage device at his young age would expose the patient to decades of cumulative risk for tube exposure or corneal endothelial decompensation. Therefore, we hoped to restore function of his natural outflow system rather than bypass it.
Advertisement
To that end, we proceeded with a 360° ab-interno trabeculotomy procedure, often referred to as a “GATT” (gonioscopy-assisted transluminal trabeculotomy.) This sutureless, blebless procedure is performed through two clear corneal paracenteses utilizing intraoperative gonioscopy. A thin, lighted catheter is inserted through a tiny paracentesis and guided through a goniotomy incision into Schlemm’s canal.
Once the catheter passes 360°, the distal end of it is retrieved from Schlemm’s, and the two ends of the catheter are pulled to tear through trabecular meshwork, completing a 360° trabeculotomy. Because this procedure augments the eye’s natural aqueous outflow rather than trying to bypass it, there is essentially no risk of hypotony, and it entails none of the long-term risk associated with implanting a drainage shunt.
Surgical time for his procedure was 12 minutes. Twenty months later, the patient’s IOP remains 8 mm Hg on dorzolamide-timolol fixed combination. In the end, we were able to achieve a durable repair of his retinal detachment and to achieve long-term control of his eye pressure with a quick, safe surgery that did not fundamentally alter his aqueous outflow physiology or ocular anatomy.
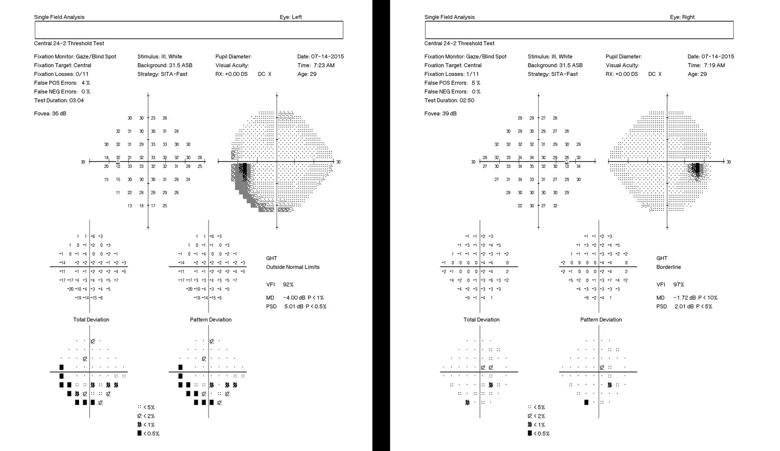
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/33c5c4d7-7ba9-4051-b919-d6cdab13f92f/18-EYE-4341-Eisengart-SMS-Study-Inset-1_jpg)
The right eye visual field is largely normal. The left field demonstrates an inferotemporal arcuate defect due to his retinal detachment.
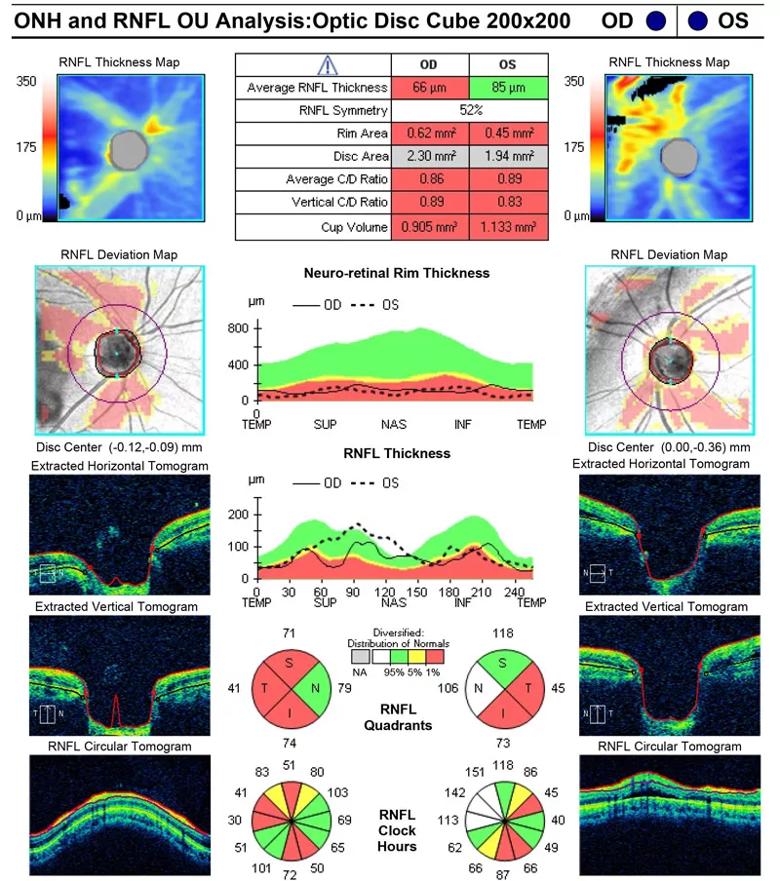
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ed0611ad-ca1f-4d71-8df0-619f62b36267/18-EYE-4341-Eisengart-SMS-Study-Inset-2_jpg)
There is diffuse retinal nerve fiber layer thinning in the right eye. Given his normal IOP and visual field, this may be physiologic. The artifactual thickening superonasally in the left eye is from intra- and subretinal fluid. Note on the ‘extracted tomograms’ at the lower left that there is subretinal fluid superonasally. Also note the large disc area OD.
Advertisement
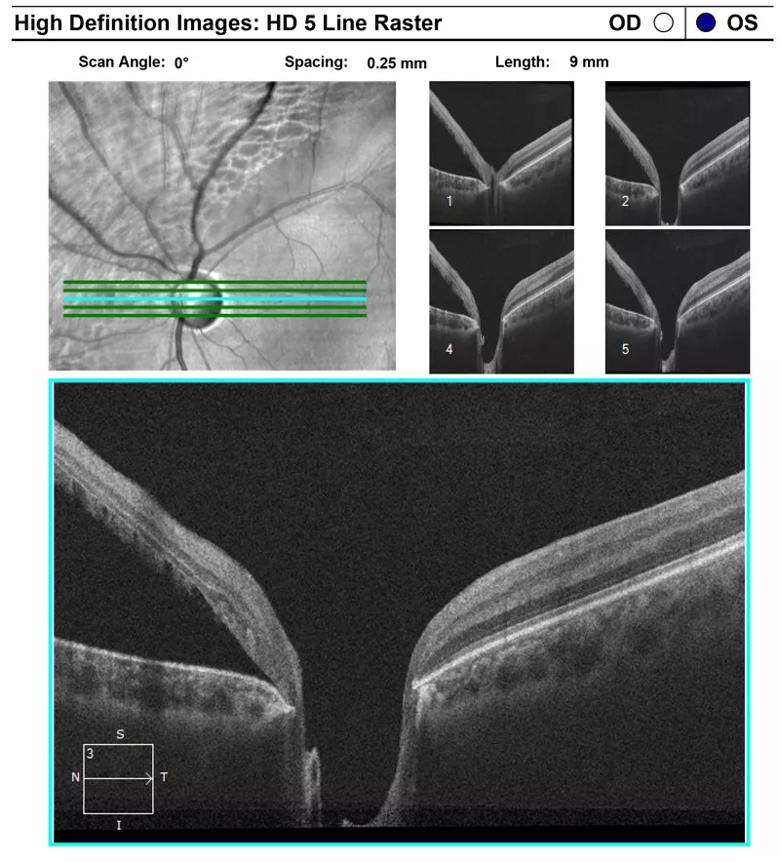
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/fb56b570-ecf8-49d9-9d6d-28698fe9539e/18-EYE-4341-Eisengart-SMS-Study-Inset-3_jpg)
A large retinal detachment is seen with subretinal fluid extending right up to the optic disc.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ceaab9ec-8a28-4e97-8fe0-5f8de36bd946/18-EYE-4341-Eisengart-SMS-Study-Hero-1_jpg)
Advertisement
Advertisement

Motion-tracking Brillouin microscopy pinpoints corneal weakness in the anterior stroma

Registry data highlight visual gains in patients with legal blindness

Prescribing eye drops is complicated by unknown risk of fetotoxicity and lack of clinical evidence

A look at emerging technology shaping retina surgery

A primer on MIGS methods and devices

7 keys to success for comprehensive ophthalmologists

Study is first to show reduction in autoimmune disease with the common diabetes and obesity drugs

Treatment options range from tetracycline injections to fat repositioning and cheek lift