Study identifies factors that may predict vision outcomes in diabetic macular edema

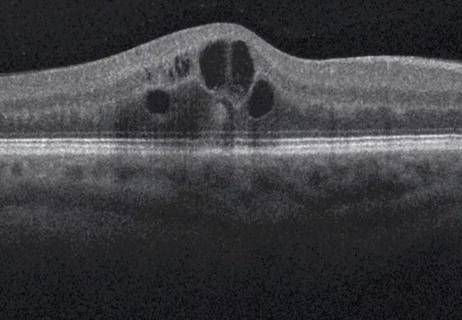
Intravitreal anti-VEGF injections are effective in controlling diabetic macular edema (DME) — at least according to clinical trials. In real-world scenarios, however, a regimen of anti-VEGF injections can increase treatment burden, leading to lapses in eye care.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The results of clinical trials, which we use to guide care, are based on patients who have a lot of resources to help them make appointments, including reminders from a research coordinator, free transportation if needed and other support as part of a research study,” says Katherine Talcott, MD, a vitreoretinal surgeon at Cleveland Clinic Cole Eye Institute. “That doesn’t reflect practice in the real world. Ophthalmology patients with advanced diabetes tend to see many specialty providers and have many healthcare appointments. They tend to be younger than other ophthalmology patients and, therefore, more likely to hold jobs and care for family members. Their lives are busy, so it’s not uncommon for them to cancel or skip eye appointments.”
Gathering data about real-world patients with DME who have lapses in anti-VEGF treatment can help inform clinical care. According to a Cleveland Clinic study published in the Journal of VitreoRetinal Diseases, certain baseline patient factors can help predict likelihood of vision loss or vision stability after a lapse in treatment.
“Better understanding the effects of treatment lapses could impact how we communicate with certain patients and tailor treatment plans,” says lead author Meghana Chalasani, MD, a Cole Eye Institute resident.
Researchers reviewed the records of 262 Cole Eye Institute patients (mean age 61) with DME who had lapses in anti-VEGF treatment of three months or longer. When they returned for care after the lapse, 61 patients had worse vision (loss in best-corrected visual acuity of at least 10 letters) while 201 had stable vision.
Advertisement
Factors associated with worse vision were:
One factor associated with stable vision was longer duration since diagnosis with diabetic retinopathy (OR of vision loss, 0.95; P < .05). This may suggest greater control of the disease before the lapse, say the authors.
Advertisement
Based on these findings, the research team developed an algorithm to predict vision outcomes in DME after lapse in anti-VEGF treatment. Due to the data collected (which more heavily represented patients with stable vision), the prediction model had a sensitivity of 20% and a specificity of 84%, making it better at predicting stable vision rather than vision loss.
“In typical case studies of patients with diabetes who have a lapse in anti-VEGF treatment, the eye disease almost always progresses, and the patient’s vision almost always worsens,” says Dr. Talcott, senior author of the study. “However, in our study, most patients with a lapse in treatment returned with stable vision.”
Ophthalmologists should not presume that DME in all patients will worsen after a lapse in anti-VEGF treatment, she notes.
Another revelation from the study is that worsening disease and treatment lapses can be associated with factors outside a patient’s control, such as insurance type.
“We need to remember that a patient’s environment and life responsibilities may be affecting their ability to maintain an eye treatment regimen,” Dr. Talcott says. “The medical community needs to be vigilant about reconnecting with these patients after a missed appointment.”
According to Dr. Chalasani, clinical responses to this study could include:
Advertisement
More research is needed to assess vision outcomes in patients who have treatment lapses after receiving newer, more durable therapies for DME.
“I’m also interested in studying the reversibility of vision loss after an anti-VEGF lapse,” Dr. Chalasani says. “Can patients regain vision if they resume a regular treatment course? And do patients who have had other interventions for diabetic retinopathy, such as panretinal photocoagulation, have added protection from losing vision after an anti-VEGF lapse?”
Adds Dr. Talcott, “We’re pleased that Meghana could publish this study as a first-year resident. Her accomplishment displays how our residents at the Cole Eye Institute balance clinical and academic work. Investing in student education, preparing young physicians to push the medical field forward, is important to Cleveland Clinic.”
Advertisement
Advertisement

Flaps, blebs and other surgical options
Greater central subfield thickness and better visual acuity at baseline are associated with longer time to resolution

Can a single subretinal injection provide effective treatment?

Innovative approach to the procedure can yield significant relief in complex cases

A scannable recap of our latest data in these clinical areas

Site visits offer firsthand lessons in clinical and operational excellence in cardiovascular care

New insights on effectiveness in patients previously treated with other anti-VEGF drugs

Evidence mounts that these diabetes and obesity drugs may protect eyes, not endanger them