Similar outcomes at lower cost than hypofractionated whole breast irradiation

It has been a debate for more than a decade: Is accelerated partial breast irradiation (APBI) as effective as hypofractionated whole breast irradiation (HWBI) in treating early-stage breast cancer? Multiple randomized trials have reported very little difference in local recurrence outcomes.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Many radiation oncologists now view the two treatments as equally effective based on NSABP B-39 and RAPID as well as previous trials,” says Chirag Shah, MD, Director of Clinical Research and Breast Radiation Oncology in Cleveland Clinic’s Department of Radiation Oncology.
But when it comes to cost, the debate continues. APBI — including advanced techniques like brachytherapy, intensity modulated radiation therapy (IMRT) and stereotactic body radiation therapy (SBRT) — is typically viewed as more expensive. The more advanced the technology, the higher the price tag, right?
Not necessarily, says Dr. Shah, whose recent study in the International Journal of Radiation Oncology • Biology • Physics (the Red Journal) compared the cost-effectiveness of image-guided APBI and HWBI after breast-conserving surgery.
“We’ve been able to show that if we use advanced technology in a way that reduces the number of treatments, the cost is less,” he says. “With image-guided APBI, we can offer outcomes comparable to whole breast irradiation with fewer side effects and at a lower cost for health systems, payers and patients.”
During the study, Dr. Shah and colleagues analyzed the cost-effectiveness of HWBI (40 Gy in 15 fractions with or without a 10-Gy/5-fraction boost) and a 30-Gy/5-fraction IMRT regimen. A 2015 randomized study in Italy already had demonstrated similar clinical outcomes and toxicities between the two techniques.
Using microcosting — evaluating detailed costs of personnel time, software, hardware and supplies — each technique was assessed a dollar amount. Indirect costs, such as patients’ travel expenses and lost work time, also were assessed.
Advertisement
The researchers found that, in women age 40 and older with low-risk breast cancer who had breast-conserving surgery, the direct cost of APBI was $1,585 less than HWBI with the boost (and $700 less without the boost). When indirect costs were included, APBI was $2,591 less than HWBI with the boost (and $1,371 less without the boost).
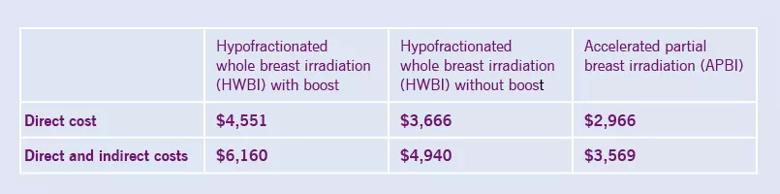
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a3be5dc5-34d5-424e-9bc5-c5bc1c8241d7/chart-inset_805x200_jpg)
In addition to being the less costly radiation therapy, APBI was found to be more effective based on quality-adjusted life years. Within 90 days of receiving breast irradiation, women receiving APBI recorded 0.2300 quality-adjusted life years compared to 0.2289 for women receiving HWBI with or without boost.
“There often is skepticism about the cost-effectiveness of new technologies,” says Dr. Shah. “Many times, payers want to know how we justify the cost and if the technique is worth it. This study showed that IMRT used for APBI is a safe and appropriate technique and can be used in a way that is value-oriented.”
That should resonate well with a healthcare industry now more focused on value-based care. With breast cancer treatment accounting for the highest amount of cancer care costs in the U.S. ($16.5 billion of the $125 billion total in 2010), IMRT APBI can offer excellent outcomes at a significant savings. According to Dr. Shah, the savings could reach $1.4 to 2.6 million (in direct and indirect costs) per 1,000 patients treated with IMRT APBI instead of HWBI.
“IMRT APBI should be considered a standard-of-care option in appropriately selected patients based on efficacy and value,” says Dr. Shah.
Advertisement
Photo Credit: Russell Lee
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient