Identifying candidates for further screening and treatment
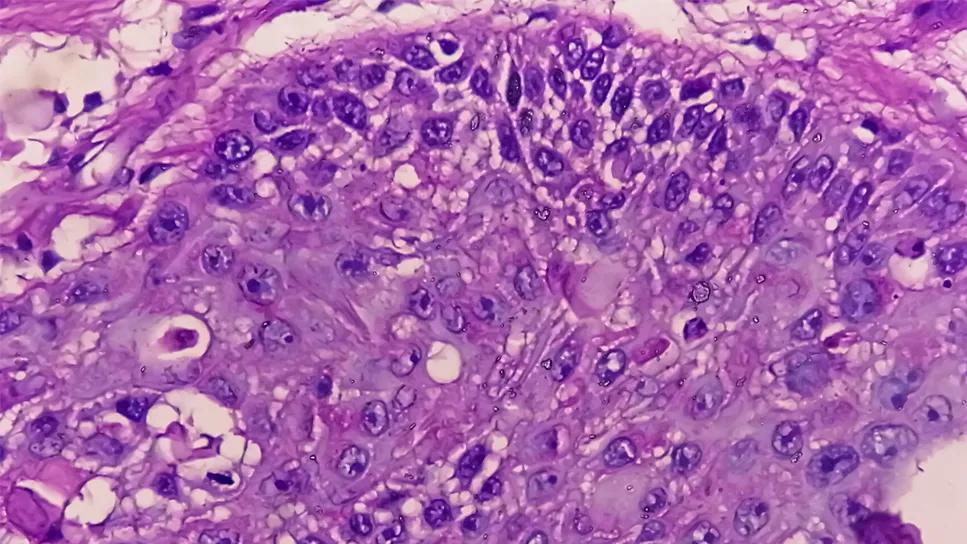
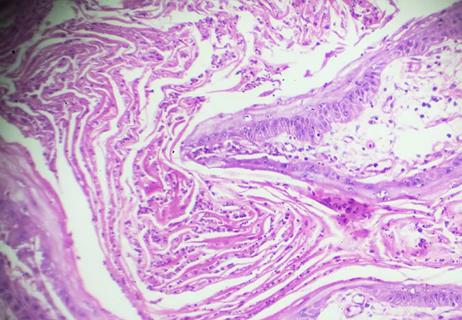
Immunosuppressed patients with lower-risk cutaneous squamous cell carcinoma (cSCC) who score higher on the 40-gene expression profile (40-GEP) biomarker test are at greater risk of recurrence, according to a study presented by Cleveland Clinic researchers at the 2024 annual conference of the American Society for Radiation Oncology.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Despite low recurrence rates overall, patients with T1-T2a cSCC can still suffer from disease recurrence and metastasis. “Surgery is often curative for cSCC, but the disease recurs in a small number of patients,” explains Shlomo Koyfman, MD, Director of the Head & Neck and Skin Cancer Radiation Oncology programs at Cleveland Clinic. “Our goal was to figure out which factors would help identify that ‘needle in a haystack’ — patients who might benefit from additional therapies. We believe our results may have implications for adjuvant radiotherapy, patient counseling, clinical trial design and post-treatment surveillance.”
cSCC is typically staged using the American Joint Commission on Cancer (AJCC) and Brigham and Women’s Hospital (BWH) tumor classification systems, and is based on tumor factors alone. Researchers at BWH and Cleveland Clinic have been working with a biosciences firm to stratify this classification system further using the DecisionDx-SCC gene expression profile test as a biomarker for recurrence.
“Although the BWH system has been available for years, our intent is to complement it with newer data,” explains Dr. Koyfman. “The preliminary data presented at ASTRO gives us a glimpse into which patients with lower-stage tumors may benefit from closer surveillance and possibly additional treatment. The hope is for these preliminary studies to help incorporate the biomarkers into the next generation of clinical trials and identify patients that may currently be appropriate for multidisciplinary evaluation.”
Advertisement
Researchers analyzed data from an independent validation cohort of 954 cSCC patients with BWH T1 and T2a tumors with definitive surgery, at least one NCCN high-risk factor and 40-GEP test results. A total of 441 patients with BWH T1 tumors and 336 patients with BWH T2a tumors were included. Two hundred eight patients were immunosuppressed, either from transplant (68.8%) or hematologic malignancies (23.1%). Less than 2% of the cohort underwent adjuvant radiotherapy. Researchers estimated and compared 3-year nodal and distant metastasis-free survival and used multivariable analysis to identify significant predictors of metastasis.
Patients with T1 tumors had similar metastasis-free survival rates regardless of immune status (P > 0.99), but when further stratified with the 40-GEP test, two distinct groups emerged (3-year metastasis-free survival: Class 1: 96.9% vs. Class 2: 88.6%, P < 0.001). Patients who were immunosuppressed with T2a tumors had significantly worse metastasis-free survival than immune-competent patients with T2a tumors (71.4% vs. 91.2%, P < 0.001) and had a higher baseline rate of NCCN very high-risk tumors (58.7% vs. 40.7%).
The 40-GEP also stratified immunosuppressed patients with T2a tumors into more favorable (Class 1: 3-yr MFS 83%) and less favorable (Class 2: 3-year MFS 57%) outcomes. Multivariate analysis demonstrated that the following were significant independent predictors of metastasis: a Class 2 40-GEP result (HR = 3.01, P < 0.001), immunosuppressed status (HR = 2.47, P < 0.001) and NCCN very high-risk rating (HR = 2.33, P = 0.002). The presence of a T2a tumor alone was not an independent predictor of metastasis (P = 0.133).
Advertisement
Why adjuvant therapy is critical for immunosuppressed patients
Dr. Koyfman’s research has shown that patients who are immunosuppressed have worse outcomes than other patients with cSCC. “One of our main therapies for recurrent cSCC is immunotherapy, which is not appropriate for many of our patients with immune suppression due to transplant, thereby rendering salvage options for recurrence more scant,” he notes. “With this biomarker, we can possibly identify patients who appear low stage but may in fact be at greater risk of recurrence. This allows for more judicious use of imaging and possibly more liberal use of adjuvant radiation than would have been recommended based on BWH tumor staging alone.”
Dr. Koyfman notes that the study findings are preliminary and that he and researchers from Brigham and Women’s Hospital are working with the biosciences firm to validate these findings on larger cohorts of data. In the interim, he argues, “maybe it’s time to use this test to determine which patients appear low stage but may warrant a closer, multidisciplinary look.”
Advertisement
Advertisement

Pembrolizumab does not improve outcomes, but immunotherapy may still offer benefit

Major study demonstrates importance of having a multidisciplinary approach to treatment for large, locally advanced tumors

Satellitosis or in-transit metastasis is a rare yet significant risk factor for this skin cancer that should be reflected in clinical staging systems.

Patient able to avoid surgery and radiation despite having rapidly growing mass
Majority of patients achieve complete pathologic response after four-dose cemiplimab therapy

Education, prevention strategies and monitoring serves this at-risk group

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting