Study associates human CD38-targeting antibody with fewer complications
The anti-cancer drug daratumumab appears to reduce the risk of major organ deterioration and hematologic disease progression in patients with immunoglobulin light-chain (AL) amyloidosis, a protein disorder that most commonly affects the heart and kidneys. According to a new study recently published in the New England Journal of Medicine, daratumumab may offer significant benefits – including a promising safety profile – when used in combination with bortezomib, cyclophosphamide and dexamethasone, a three-drug regimen frequently used to treat multiple myeloma.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
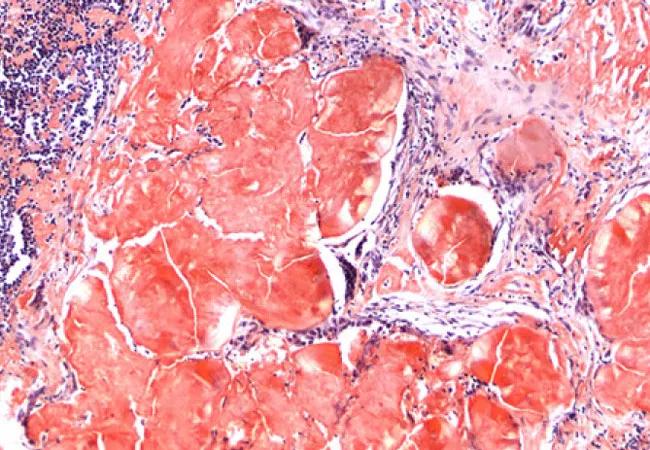
AL amyloidosis is commonly managed with bortezomib-based chemotherapy, but there is room for improvement in prolonging the survival of these patients. Researchers in the multicenter phase III ANDROMEDA clinical trial evaluated whether the addition of daratumumab, a fully humanized CD38-targeting antibody, could improve outcomes in patients with the disease, which is characterized by the deposition of amyloid fibrils of light chains produced by clonal CD38+ plasma cells.
The outlook for patients with AL amyloidosis has improved in recent years thanks to novel chemotherapy treatments and better patient selection for high-dose melphalan and autologous stem cell transplantation. However, the disease has remained particularly challenging to diagnose and manage, and outcomes have historically been bleak.
“A deep, rapid hematologic response is essential to the survival of patients with AL amyloidosis,” explains Jason Valent, MD, study co-author and oncologist in the Taussig Cancer Institute at Cleveland Clinic. “Unfortunately, the disease is already advanced by the time we see most of these cases, a reality that limits our treatment options and ability to improve long-term survival. Although targeted chemotherapy is the best way we’ve had to prevent the progressive disability and death that results from multiorgan involvement, the rate of hematologic complete response in these patients has been suboptimal. Now, however, there is good evidence that daratumumab as an adjunct to conventional therapies may improve organ function and survival.”
Advertisement
A total of 388 patients with newly diagnosed AL amyloidosis were randomized to receive six cycles of bortezomib, cyclophosphamide and dexamethasone either alone or with subcutaneous daratumumab, followed by single-agent daratumumab every four weeks for up to 24 cycles in the patients treated with daratumumab. The primary end point was a hematologic complete response.
The percentage of patients who had a hematologic complete response was significantly higher in the daratumumab group than in the control group (53.3% vs. 18.1%). Survival free from major organ deterioration or hematologic progression significantly favored the daratumumab group (hazard ratio for major organ deterioration, hematologic progression or death, 0.58; 95% CI, 0.36 to 0.93; P = 0.02). At six months, more cardiac and renal responses occurred in the daratumumab group than in the control group (41.5% vs. 22.2% and 53.0% vs. 23.9%, respectively).
The four most common grade 3 or 4 adverse events were lymphopenia (13.0% in the daratumumab group and 10.1% in the control group), pneumonia (7.8% and 4.3%, respectively), cardiac failure (6.2% and 4.8%) and diarrhea (5.7% and 3.7%). Systemic administration-related reactions to daratumumab occurred in 7.3% of study subjects. A total of 56 patients died (27 in the daratumumab group and 29 in the control group), most due to amyloidosis-related cardiomyopathy. Serious adverse events, most commonly pneumonia, occurred in 43.0% of those in the daratumumab group and 36.2% of those in the control group.
Advertisement
Survival free from major organ deterioration, hematologic progression or subsequent treatment was superior in the daratumumab group, as was the percentage of patients who experienced a cardiac or renal response.
“This is an important finding given that organ responses are objective measures of clinically relevant and observable end points for patients with AL amyloidosis as well as predictors of improved survival,” notes Valent.
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient