Dr. Robert Fox puts a tissue marker study in context
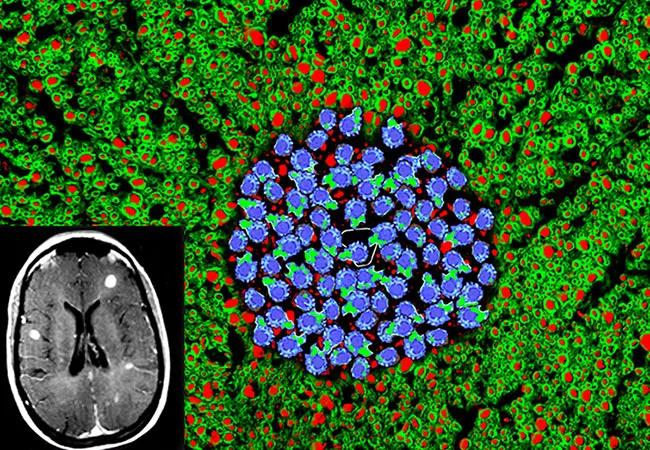
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5bc1ecf8-36f6-4b89-a013-9a8d2de17027/16-NEU-2602-Trapp-650x450_jpg)
16-neu-2602-trapp-650×450
Treatment of relapsing-remitting multiple sclerosis (MS) in 2018 remains far from what can be described as personalized medicine, but an important initial step toward more personalized management of MS relapses has been achieved by researchers with University Medical Center Goettingen in Germany. So contends Cleveland Clinic neurologist Robert Fox, MD, in an editorial accompanying the German study published online by JAMA Neurology on February 5, 2018.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The retrospective cohort study evaluated the response to apheresis in relation to histopathologically defined immunopathological patterns of MS in 69 patients. As detailed in the published study report, the investigation provides the first evidence that short-term treatment response is related to the underlying inflammatory pathology within MS lesions.
“These observations further support the clinical relevance of MS lesion patterns and suggest that they may be useful in better understanding the heterogeneity in treatment response to MS therapies,” Dr. Fox writes in his editorial. He adds that the study is also helpful in providing further evidence supporting apheresis as short-term therapy for central nervous system demyelination.
At the same time, he notes, the study’s applicability is limited by the fact that all 69 patients underwent brain biopsy, which is highly unusual and invasive for MS patients in real-world practice. “The future of personalized medicine in MS requires markers that are easily obtained and measured,” Dr. Fox writes, citing fluid or imaging biomarkers as examples. Until such markers are identified, the tissue markers from the current study will remain only a research tool for the occasional patient who requires a brain biopsy.
The full Fox editorial is available here, and the Goettingen researchers’ study is available here.
Advertisement
Advertisement
Guidance from the largest cohort of SEEG-confirmed insular epilepsy patients reported to date
Ethical guidance provides guardrails so medical advances benefit patients
OCEANIC-STROKE results represent long-sought advance in secondary stroke prevention
Two studies from Cleveland Clinic may help advance the technology toward broader clinical use
Distinct MRI signature includes lesions beyond the corpus callosum, features predictive of vision and hearing loss
An argument for clarifying the nomenclature
An expert talks through the benefits, limits and unresolved questions of an evolving technology
Recommendations on identifying and managing neurodevelopmental and related challenges