Advanced radiotherapy in a rare soft-tissue sarcoma
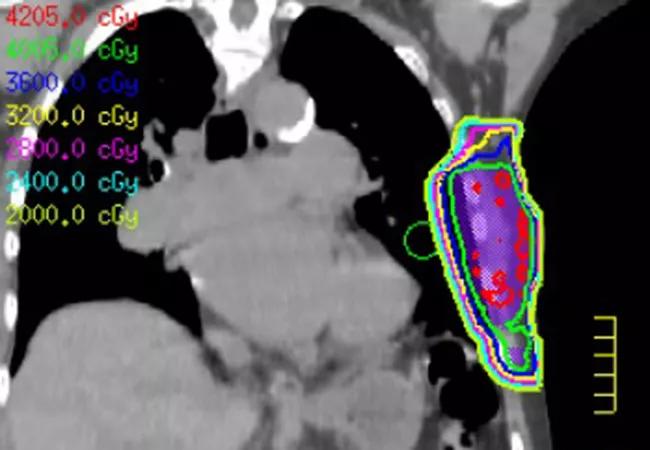
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/4ed2cf6b-55a4-4d06-86a5-36d5ab35df71/650x450_Chest-Wall-Sarcoma_jpg)
650x450_Chest-Wall-Sarcoma
A patient in whom radiation both cured breast cancer and caused heart disease — necessitating a transplant — presents 25 years after initial radiotherapy with a mass on her left chest wall above her transplanted heart.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“When we diagnose patients like this with chest wall sarcomas, they are often surprised to hear that radiotherapy is part of the answer, though initial radiation may have contributed to the current cancer’s development,” says Chirag Shah, MD, Director of Clinical Research, Radiation Oncology, Cleveland Clinic. “With advanced techniques, we can often treat these rare cancers.”
Primary soft tissue sarcomas (STS) of the chest wall are rare, accounting for less than 5% of all thoracic malignancies, and can be difficult to treat. “We see them most often in women who have had radiation for breast cancer or for Hodgkin’s lymphoma,” says Dale Shepard, MD, PhD, Co-Director of Cleveland Clinic Cancer Center’s Rare Cancer and Blood Disease Program. “But we also see patients with no history of cancer or radiation therapy.”
Breast cancer and Hodgkin’s survivors who develop radiation-induced chest wall sarcomas are often told that they have few options because they cannot have radiation again. Cleveland Clinic’s Rare Cancer and Blood Disease Program, however, is designed to help such patients by giving them the collective expertise of dozens of specialists who study, diagnose and treat uncommon diseases on a regular basis.
A recent review of 192 patients with chest wall sarcomas found that five and 10-year survival rates were 73% and 61%, respectively, with a median survival of 14 years. Symptoms can include a mass or pain or nothing at all, with the tumor discovered upon routine chest radiograph. Distinguishing from Ewing sarcoma and osteosarcoma with core needle biopsy is critical given the different treatment approaches.
Advertisement
In the case of radiation-induced chest wall sarcomas, the malignancy may not develop until 20 to 25 years after the original cancer was treated. “It can even happen after a mastectomy,” says Dr. Shah, “but it often happens deep in the chest wall so sometimes it’s not something that can be seen by the naked eye or felt on a physical exam early on.”
In the case of this breast cancer survivor with a heart transplant, physicians were able to give her targeted radiation and then remove the mass with negative margins.
“In this patient, and in many other patients we treat with chest wall sarcoma, we used a variety of techniques, including brachytherapy,” says Dr. Shah. Very few centers in the U.S. offer brachytherapy for chest wall sarcomas, and Dr. Shah and Jacob Scott, MD, DPhil, were recently co-authors on national guidelines regarding this technique.
“We also incorporate various cardiac- and lung-sparing techniques, including the use of deep inspiratory breath hold during treatment planning, an active breathing control system during daily treatment and heart blocks.” The team is preparing data for publication showing that cardiac doses at Cleveland Clinic are lower than the national standard by more than 50 percent.
“If you exclude the most complicated cases treating targets near the heart, the average is closer to a 75 percent reduction,” says Dr. Shah. “We’re really proud of what we’ve been able to achieve for our patients using a combination of cardiac-sparing techniques.”
Because chest wall sarcomas are so challenging to treat, physicians with Cleveland Clinic’s Rare Cancer and Blood Disease Program use an interdisciplinary approach that involves thoracic surgery, plastic surgery, medical oncology and radiation oncology.
Advertisement
“Before we even start treatment, we meet as a group and plan it out,” says Dr. Shah. “Everything has to be coordinated very carefully. Before we offer treatment, we’ll discuss the case, review the imaging and talk about how to best sequence things. Most of the time that’s radiation followed by surgery but sometimes it’s actually surgery followed by radiation. It’s a discussion of what’s best for the patient and what surgical and reconstructive approach will be.”
Advertisement
Advertisement
Goal-of-care discussions drive earlier hospice access
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting