Study finds strong association between brain/thalamic volume and T2 lesion volume
Whole brain and deep gray matter atrophy correlates more strongly with clinical disability than does T2 lesion volume (T2LV) in individuals with multiple sclerosis (MS), according to a Cleveland Clinic platform presentation at the American Academy of Neurology’s 2019 annual meeting on May 7.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The study — led by neuroimmunologist Kedar Mahajan, MD, PhD, in collaboration with staff scientist Kunio Nakamura, PhD, of Cleveland Clinic’s Department of Biomedical Engineering — shines new light on the relevance of deep gray matter atrophy in MS.
“Developing new biomarkers of inflammatory disease activity has long been at the forefront of clinical research efforts,” says Dr. Mahajan, a staff physician in Cleveland Clinic’s Mellen Center for Multiple Sclerosis Treatment and Research. “Our findings indicate that brain and thalamic volume should continue to be used as outcomes in clinical trials of MS and that additional work is needed to apply these tools in clinical practice.”
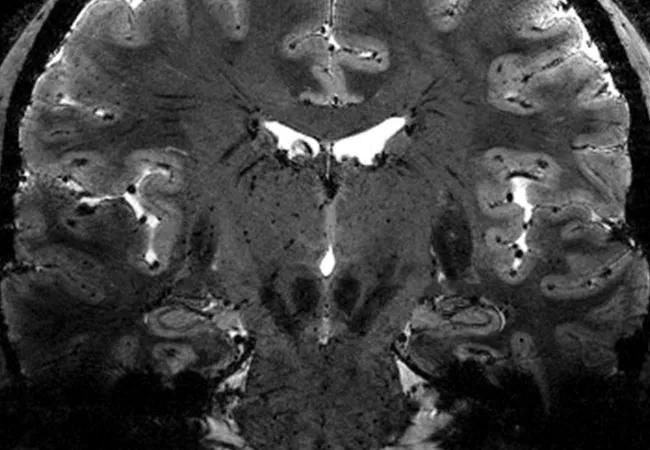
Neurologists routinely use MRI to track disease activity in patients with MS. On average, approximately 10 new/enlarging white matter inflammatory lesions are discovered for each clinical relapse.
However, Dr. Mahajan notes, there is an underappreciated process of neurodegeneration that occurs independent of the development of new inflammatory lesions. Because gray matter atrophy occurs very early in the disease process, it may be a suitable early predictor of worsening disability in MS.
“The goal of our study was to identify advanced imaging markers that can best reflect this neurodegeneration and clinical worsening of disability, with the hope of translating the findings to clinical practice,” he says. “Specifically, we wanted to investigate whether T2LV correlates with thalamic atrophy in a large real-world dataset from a tertiary referral/comprehensive center for MS.”
Advertisement
The study was inspired by previous research using Cleveland Clinic’s postmortem rapid autopsy program for patients with MS, which has shown that lesions in the thalamus do not correlate with thalamic atrophy but that lesions throughout the brain do impact its volume. The current study is distinctive because it included a large number of patients and used real-world data rather than data from a clinical trial setting.
Clinical neuroperformance data, demographic and disease characteristics, and patient-reported outcomes were obtained from 997 patients with MS during routine clinical care. MRI brain volumes were analyzed in Dr. Nakamura’s lab for T2LV, whole brain fraction and deep gray matter volumes (thalamus, putamen, caudate and hippocampus). Associations were assessed using Spearman correlation coefficients with significance set at P < 0.001.
Significant associations were found between T2LV and each of the following:
There was no association between T2LV and caudate volume. Whole brain volume was identified as the strongest predictor of thalamic volume.
“Our findings indicate that new/enlarging T2 lesions can have secondary effects and cause damage to the brain through transsynaptic injury,” says Dr. Mahajan. “This means that a lesion in one spot can impact the brain volume of a structure that it projects to. As a result, effects may be exerted on the brain that are not necessarily caused by the lesion(s) alone.”
Advertisement
Furthermore, he notes, a drug’s effect on brain and thalamic volume could impact the choice of MS therapies as well as the development of new therapies.
“If you have drug A that slows the rate of brain/thalamic atrophy more than drug B does, in addition to stopping clinical attacks and new lesions, then this should influence the choice of therapy,” he explains. “Biomarkers such as brain and thalamic volume could also have utility in the development of new therapies aimed at repairing or providing protection from primary and secondary neurodegeneration. Certain therapies may change the trajectory of atrophy by reducing the annualized atrophy rate relative to others.”
As a follow-up to the current study, Dr. Mahajan’s team plans to integrate their data with data obtained by other institutions participating in the MS PATHS (MS Partners Advancing Technology and Solutions) collaborative project, of which Cleveland Clinic is one of the founding members.
“We plan to extend this work to the larger MS PATHS dataset and look at longitudinal data to see how the accrual of new/enlarging T2 lesions impacts brain and deep gray matter volume,” he says. “We also plan to use advanced MRI techniques to investigate how lesions along certain thalamic projections impact volumes of individual thalamic nuclei.”
Additionally, Dr. Mahajan is collaborating with the laboratory of Bruce Trapp, PhD, of the Department of Neurosciences on a related ongoing project that utilizes Cleveland Clinic’s rapid autopsy program to understand the pathologic changes in patients with increased thalamic atrophy.
Advertisement
Advertisement

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Tool helps patients understand when to ask for help