Urologists describe outcomes and techniques for promising, new approach
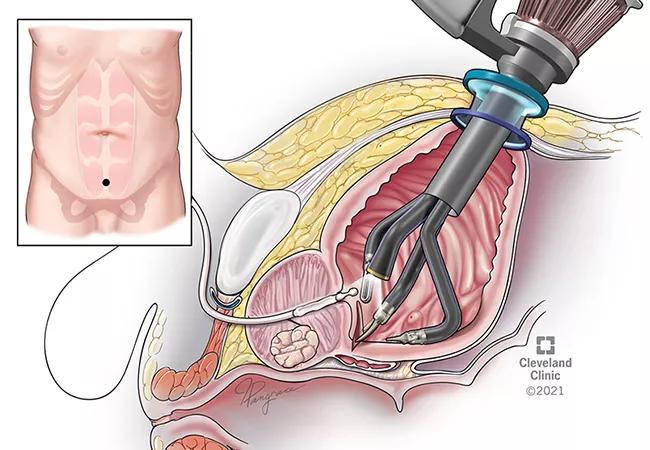
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/bfd4a2ee-4189-4f9c-926f-2d98a3f5c09b/22-URL-2979922-B-CQD-650x450-1_jpg)
R-Port Laparoscopic Trans BladderProstatectomy
In urologic surgery, the combination of the single-port (SP) robot and the transvesical technique, or surgical access to the prostate directly through the bladder, is providing excellent results, rapid recovery and improved patient satisfaction.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Usually innovation goes hand-in-hand with technological and surgical skills advancement, says Jihad Kaouk, MD, Director of the Center for Robotic and Image-Guided Surgery at the Glickman Urological & Kidney Institute.
Under the direction of Dr. Kaouk, Cleveland Clinic has a long list of achievements in urologic robotic surgery. Over the last several years, the team has used the SP robotic system to assist with kidney transplant and autotransplant, nephrectomy, pyeloplasty, prostate surgery, including prostatectomy, cystectomy, and urinary tract reconstruction.
“Using the SP robot with the transvesical approach allows us to go directly into the bladder, this means that we avoid the intraperitoneal cavity, which is not feasible with the multiport approach. This has led to less pain and postoperative ileus because the bowels stay intact,” says Dr. Kaouk.
The technique and comparative outcomes studies drew attention this year at the American Urological Association annual meeting in New Orleans.
Mahmoud Abou Zeinab, MD, a research fellow in the Department of Urology, presented findings from a prospective, multicenter trial that examined perioperative outcomes from 91 patients undergoing SP transvesical prostatectomy versus 201 undergoing multiport (MP) robotic simple prostatectomy.
“Notably, we found that SP transvesical patients were more likely to be discharged the same day of surgery and with a lower pain score. Although intraoperative and postoperative complication rates were similar, readmission was higher in the MP cohort,” he notes. “We believe in experienced hands, SP simple prostatectomy is a good alternative to the MP approach.”
Advertisement
He presented a step-by-step approach of the procedure in the video below, sharing insights on a particularly complex case involving a large median lobe.
Video content: This video is available to watch online.
View video online (https://www.youtube.com/embed/pSzCB7NpY-0?feature=oembed)
Single-Port Transvesical Simple Prostatectomy For Big Median Lobe (Graphic)
Since November 2020, the Cleveland Clinic team has performed around 125 transvesical robot-assisted radical prostatectomies (RARP). In 2021, Dr. Kaouk and colleagues were the first to report their experience and early outcomes of this technique for radical prostatectomy and pelvic node dissection. Several comparative studies are now underway and will soon publish.
“We first used this approach as an alternative to avoid a hostile abdomen in patients with previous and extensive abdominal surgeries and scarring,” says Dr. Kaouk. Patients with ulcerative colitis, Crohn’s disease, or those who have had a proctocolectomy are not candidates for other approaches, he explains.
Now, it’s becoming a preferred option for select patients with low- to intermediate-risk prostate cancer, notes Dr. Kaouk.
Early results demonstrated a significant impact on urine control (50% had immediate continence), short postoperative Foley duration (3 days post-surgery), minimal perioperative complications, limited use of opioids for pain control, low risk for transfusion (none reported so far), and fast recovery, with about 87% of patients in an outpatient setting within 4 hours of surgery.
Alp Tuna Beksac, MD, a fellow in the Department of Urology, presented the following step-by-step instruction of the technique at the AUA meeting.
Video content: This video is available to watch online.
View video online (https://www.youtube.com/embed/1d27We3E0V8?feature=oembed)
Single-Port Transvesical Robotic Radical Prostatectomy: Step by Step Description (Graphic)
Dr. Kaouk concludes, “We focus on innovations that bring value to the patient with a less invasive procedure, to the surgeon by providing more surgical options and tools to serve their patients, and to the health system by moving more surgeries to an outpatient setting to serve more patients with the existing limited number of inpatient units.”
Advertisement
Advertisement
Pediatric urologists lead quality improvement initiative, author systemwide guideline
Fixed-dose single-pill combinations and future therapies
Reproductive urologists publish a contemporary review to guide practice
Two recent cases show favorable pain and cosmesis outcomes
Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood
Proteinuria reduction remains the most important treatment target.
IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy
Oncologic and functional outcomes are promising, but selection is key