Newer procedure is proving successful for certain patients
Interventional pain management specialists at Cleveland Clinic have begun performing a minimally invasive procedure that is bringing long-term relief to patients with chronic lower back pain (CLBP) for whom standard medical care has not yielded durable results.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The new intraosseous nerve-ablating procedure, known commercially as the Intracept® System, targets the basivertebral nerve of the vertebral endplate, the region that serves as an interface between the vertebra and the disk.
A multicenter study of 225 patients randomized to treatment (147) or sham (78) interventions reported in the International Journal of Spine Surgery showed sustained clinical benefits on both the Oswestry Disability Index (ODI) and the Visual Analog Scale (VAS) as well as high responder rates at 2 years following treatment. Mean percent improvements in ODI and VAS compared to baseline were 54% and 53%, respectively, in patients who had the procedure.
Suboptimal success rates with conventional treatments for CLBP have led medical researchers to probe whether they have been missing a pain generator. Anatomic studies over the past several years have shown the vertebral endplates to be a significant source of CLBP.
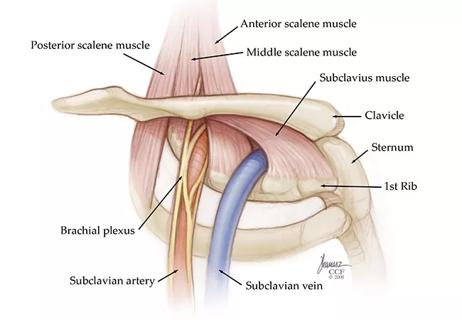
The vertebral endplates contain a rich nerve supply stemming from the basivertebral nerve that transmits pain from the superior and inferior endplates. Studies have found that there are endplate changes associated with disk degeneration. Basivertebral nerve density has been found to be higher in endplate regions that have been damaged, indicating a connection between these nerves and CLBP.
“A large number of patients are refractory to conventional pain measures, including steroid injections and medications,” explains Cleveland Clinic Pain Management specialist Sherif Costandi, MD, who is performing the new procedure and seeing success. “Despite what we do for them, these patients get no relief or only short-term or partial relief, and then end up having surgery. However, surgery also provides limited relief in many cases, and can even make the pain worse.”
Advertisement
Dr. Costandi says the identification of the vertebral endplates and the basivertebral nerve as the source of pain for many CLBP patients may help explain why these standard procedures and surgical interventions have produced mixed results.
Performed on an outpatient basis, Intracept uses fluoroscopic guidance to introduce a cannula through the pedicle. A curved cannula is employed to create a channel to the trunk of the basivertebral nerve. A radiofrequency probe is inserted and placed at the nerve, which is ablated using a radiofrequency generator.
Candidates for Intracept include patients with CLBP whose pain has not responded to conventional measures, including all medications used to treat CLBP, for at least six months. Patients must show evidence on MRI of type 1 or type 2 Modic changes, including inflammation, edema, endplate changes, disruption and fissuring of the endplate, vascularized fibrous tissues within the adjacent marrow, hypointensive signals (type 1) or changes to the vertebral body marrow, including replacement of normal bone marrow by fat, and hyperintensive signals (type 2).
Contraindications for Intracept include severe osteoporosis, a spinal infection, severe cardiac or pulmonary compromise, the presence of an implantable pulse generator or other electronic implant, skeletal immaturity and pregnancy. It is not yet known whether patients who have received conventional surgery for CLBP with limited results are candidates for Intracept.
“Though this procedure is not the first course of treatment for patients with CLBP, it offers a safe and effective therapeutic tool for individuals who’ve suffered for months with little or no response to conservative care and have type 1 or type 2 Modic changes on their spine MRI,” Dr. Costandi says.
Advertisement
Advertisement

Researchers seek solutions to siloed care, missed diagnoses and limited access to trauma-informed therapies

Study participants also reported better sleep quality and reduced use of pain medications

Two-hour training helps patients expand skills that return a sense of control

Program enhances cooperation between traditional and non-pharmacologic care

National Institutes of Health grant supports Cleveland Clinic study of first mechanism-guided therapy for CRPS
Pain specialists can play a role in identifying surgical candidates

Individual needs should be matched to technological features

New technologies and tools offer hope for fuller understanding