Effective therapy is available, but underutilized
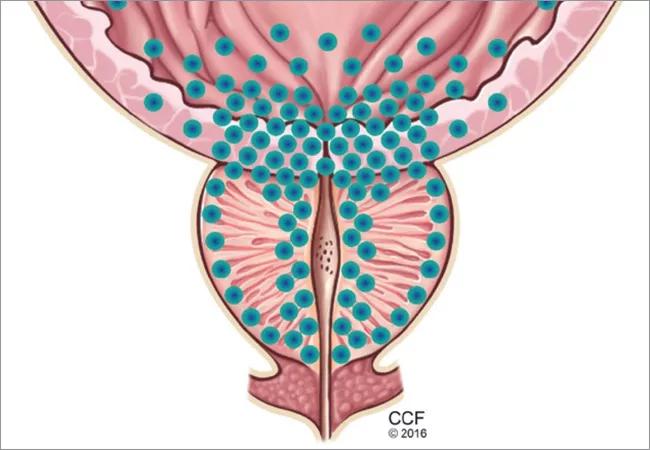
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/caf29816-2ec7-4f5b-895d-1c4fccf0c293/650x450-BPH_jpg)
650×450-BPH
By Raman Unnikrishnan, MD; Nima Almassi, MD; and Khaled Fareed, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
(This post is an abridged version of a January 2017 Cleveland Clinic Journal of Medicine article.)
Primary care physicians are uniquely positioned to screen for benign prostatic hyperplasia (BPH) and lower urinary tract symptoms, to perform the initial diagnostic workup and to start medical therapy in uncomplicated cases. Effective medical therapy is available but underutilized in the primary care setting.
This overview covers how to identify and evaluate patients with lower urinary tract symptoms, initiate therapy and identify factors warranting timely urology referral.
BPH is a histologic diagnosis of proliferation of smooth muscle, epithelium, and stromal cells within the transition zone of the prostate, which surrounds the proximal urethra.
Symptoms arise through two mechanisms: static, in which the hyperplastic prostatic tissue compresses the urethra (Figure 1); and dynamic, with increased adrenergic nervous system and prostatic smooth muscle tone (Figure 2). Both mechanisms increase resistance to urinary flow at the level of the bladder outlet. As an adaptive change to overcome outlet resistance and maintain urinary flow, the detrusor muscles undergo hypertrophy. However, over time the bladder may develop diminished compliance and increased detrusor activity, causing symptoms such as urinary frequency and urgency. Chronic bladder outlet obstruction can lead to bladder decompensation and detrusor underactivity, manifesting as incomplete emptying, urinary hesitancy, intermittency (starting and stopping while voiding), a weakened urinary stream and urinary retention.
Advertisement
Figure 1. The static component of benign prostatic hyperplasia and lower urinary tract symptoms, with hyperplasia leading to urethral compression.
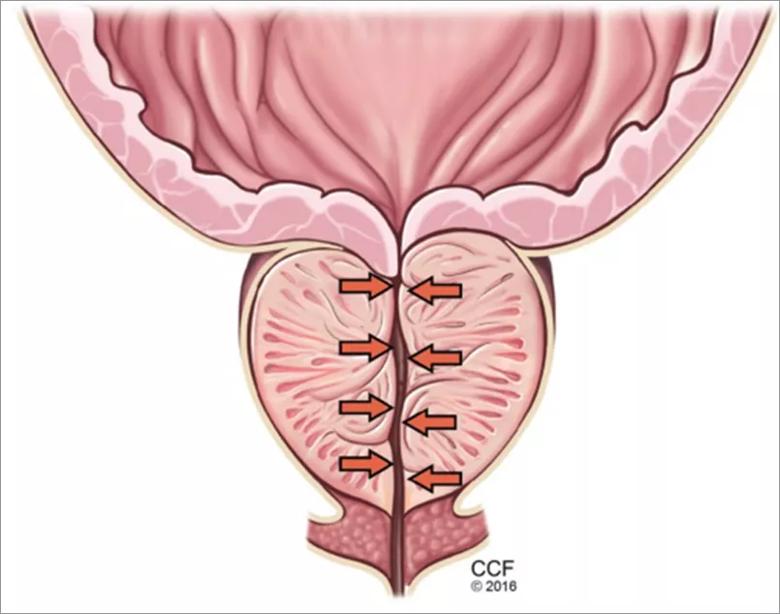
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3baab29b-dca7-49c5-af06-3a281d087c6e/Figure-1_jpg)
Figure 2. The dynamic component of benign prostatic hyperplasia. The bladder outlet and prostate are richly supplied with alpha-1 receptors (their distribution represented by blue dots), which increase smooth muscle tone, promoting obstruction to the flow of urine. Alpha-1 adrenergic blockers counteract this effect.
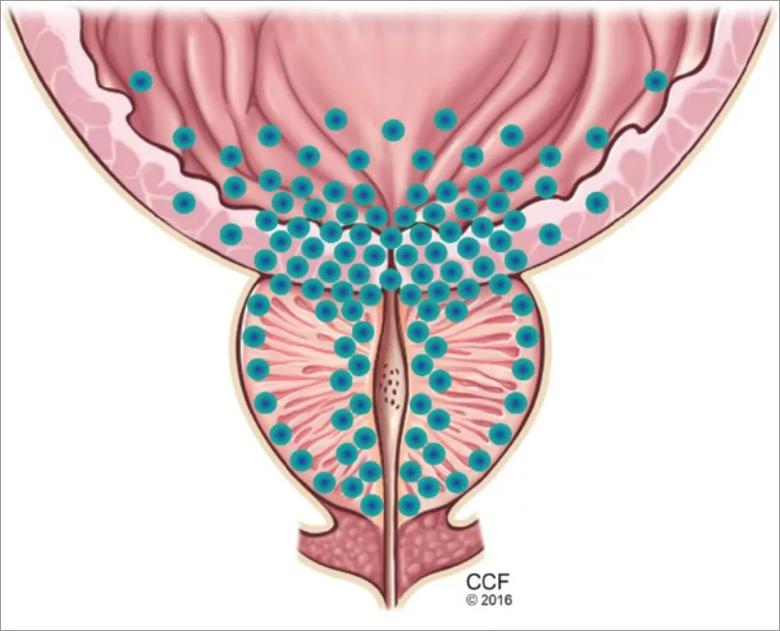
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8461c807-9ef0-46f8-918a-056ce57d064f/Figure-2_jpg)
Autopsy studies have shown that BPH increases in prevalence with age beginning around age 30 and reaching a peak prevalence of 88 percent in men in their 80s. This trend parallels those of the incidence and severity of lower urinary tract symptoms. In the year 2000 alone, BPH was responsible for 4.5 million physician visits at an estimated direct cost of $1.1 billion, not including the cost of pharmacotherapy.
BPH can cause lower urinary tract symptoms that fall into two categories: storage and emptying. Storage symptoms include urinary frequency, urgency and nocturia, whereas emptying symptoms include weak stream, hesitancy, intermittency, incomplete emptying, straining and postvoid dribbling.
Assessment begins with characterizing the patient’s symptoms and determining those that are most bothersome. Because BPH is just one of many possible causes of lower urinary tract symptoms, a detailed medical history is necessary to evaluate for other conditions that may cause lower urinary tract dysfunction or complicate its treatment.
Advertisement
A general examination should include the following:
All men with lower urinary tract symptoms should complete the International Prostate Symptom Score (IPSS) survey, consisting of seven questions about urinary symptoms plus one about quality of life. Specifically, it asks the patient, “Over the past month, how often have you….”
Advertisement
Scores are categorized as mild, moderate and severe. The questionnaire can also be used to evaluate for disease progression and response to treatment over time.
Urinalysis is recommended to assess for urinary tract infection, hematuria, proteinuria or glucosuria.
A fluid diary is useful for patients complaining of frequency or nocturia and can help quantify the volume of fluid intake, frequency of urination and volumes voided. The patient should complete the diary over a 24-hour period, recording the time and volume of fluid intake and each void.
Measuring serum creatinine is not recommended in the initial BPH workup, as men at higher risk of renal failure than those without these symptoms.
Prostate-specifi c antigen (PSA) utility extends to guiding the management of BPH. PSA levels correlate with prostate volume and subsequent growth.
In addition, the risks of developing acute urinary retention or needing surgical intervention rise with increasing PSA. Therefore, men with BPH and an elevated PSA are at higher risk with watchful waiting and may be better served with medical therapy.
If the initial evaluation reveals hematuria, recurrent urinary tract infection, a palpable bladder, abnormal findings on digital rectal examination suggesting prostate cancer, or a history of or risk factors for urethral stricture or neurologic disease, the patient should be referred to a urologist for further evaluation (Table 1). Other patients who should undergo urologic evaluation are those with persistent bothersome symptoms after basic management and those who desire referral.
Advertisement
TABLE 1
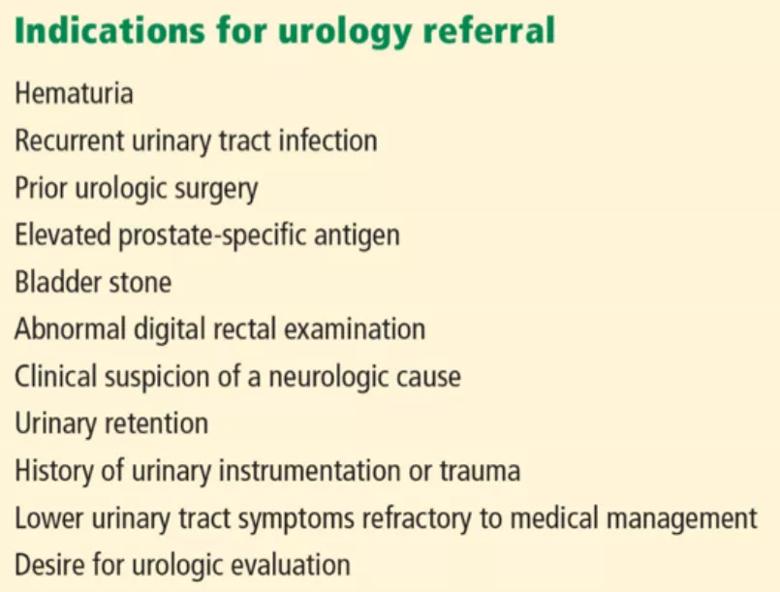
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1e30c5e1-f914-43b8-955d-c17dbc617e88/Table-1_jpg)
Patients referred for urologic evaluation may require additional tests for diagnosis and to guide management.
While BPH is rarely life-threatening, it can significantly detract from a patient’s quality of life. The goal of treatment is not only to alleviate bothersome symptoms, but also to prevent disease progression and disease-related complications.
Understanding the natural history of BPH is imperative to appropriately counsel patients on management options, which include
Though men managed with watchful waiting are at no higher risk of death or renal failure than men managed surgically, population-based studies have demonstrated an overall risk of acute urinary retention of 6.8/1,000 person-years with watchful waiting. Older men with a larger prostate, higher symptom score, and lower peak urinary flow rate are at higher risk of acute urinary retention and progression to needing BPH treatment.
There is evidence that patients progressing to needing surgery after an initial period of watchful waiting have worse surgical outcomes than men managed surgically at the onset. This observation must be considered in counseling and selecting patients for watchful waiting. Ideal candidates include patients who have mild or moderate symptoms that cause little bother. Patients electing watchful waiting warrant annual follow-up including history, physical examination, and symptom assessment with the International Prostate Symptom Score (IPSS) survey.
Behavioral modification should be incorporated into whichever management strategy a patient elects. Such modifications include:
Drugs for BPH include alpha-adrenergic blockers, 5-alpha reductase inhibitors, anticholinergics, beta-3 agonists, and phosphodiesterase-5 inhibitors.
In clinical trials in BPH, alpha-blockers improved the symptom score by 30 percent to 45 percent and increased the peak urinary flow rate by 15 percent to 30 percent from baseline values. These agents have a rapid onset (within a few days) and result in significant symptom improvement. They are all about the same in efficacy (Table 2), with no strong evidence that any one of them is superior to another.
TABLE 2
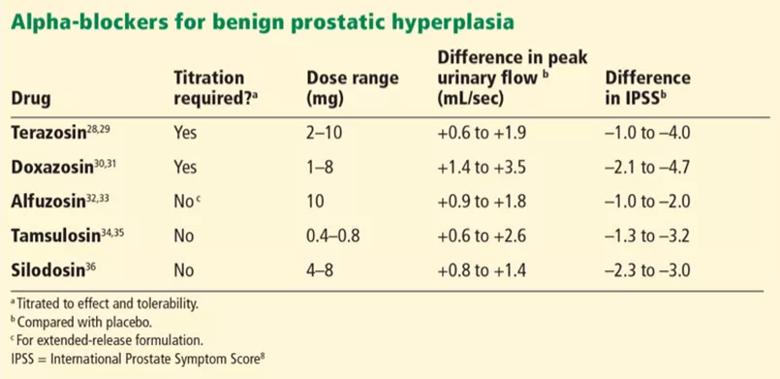
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/04b882c4-8e05-437d-b5e7-d9fc75a6fa6c/Table-2_jpg)
Though rapidly effective in reducing symptoms, alpha-blocker monotherapy may not be the best option in men at higher risk of BPH progression, as discussed below.
Before starting this therapy, patients must be counseled about common side effects such as dizziness, fatigue, peripheral edema, orthostatic hypotension and ejaculatory dysfunction.
To maximize efficacy of alpha-blocker therapy, it is imperative to understand dosing variations among agents. Alpha-blocker therapy should be delayed in patients planning to undergo cataract surgery.
There are also two 5-alpha reductase inhibitors: dutasteride and finasteride. Both agents induce apoptosis of prostatic stroma, with a resultant 20 percent to 25 percent mean reduction in prostate volume.
Finasteride and dutasteride are believed to mitigate the static obstructive component of BPH, with similar improvements in urinary flow rate (1.6–2.2 mL/sec) and symptom score (–2.7 to – 4.5 points) in men with an enlarged prostate. Indeed, data from the MTOPS trial showed that men with a prostate volume of 30 grams or greater or a PSA level of 1.5 ng/mL or greater are most likely to benefit from 5-alpha reductase inhibitors. Maximum symptomatic improvement is seen after 3 to 6 months of 5-alpha reductase inhibitor therapy.
In addition to improving urinary flow and lower urinary tract symptoms, finasteride has been shown to reduce the risk of disease progression in men with prostates greater than 30 grams.
Before starting 5-alpha reductase inhibitor therapy, patients should be counseled about common adverse effects such as erectile dysfunction (occurring in 5-8 percent), decreased libido (5 percent), ejaculatory dysfunction (1-5 percent) and gynecomastia (1 percent).
Given its superior efficacy and benefits in preventing disease progression, combination therapy (the alpha-blocker, doxazosin, and the 5-Alpha reductase inhibitor, finasteride) should be considered for men with an enlarged prostate and moderate to severe lower urinary tract symptoms.
Anticholinergics were historically contraindicated in men with BPH because of concern about urinary retention. However, in men with a postvoid residual volume less than 200 mL, anticholinergics do not increase the risk of urinary retention. Further, greater symptom improvement has been demonstrated with the addition of anticholinergics to alpha-blocker therapy for men with BPH, irritative lower urinary tract symptoms, and a low postvoid residual volume.
An alternative to anticholinergic agents is the beta-3 agonist mirabegron. Mirabegron does not have anticholinergic side effects and is generally well tolerated, though poorly controlled hypertension is a contraindication to its use.
Phosphodiesterase-5 (PDE5) inhibitors, a mainstay in the treatment of erectile dysfunction, have demonstrated significant improvement in lower urinary tract symptoms with an average two-point IPSS improvement on a PDE5 inhibitor compared with placebo.
Tadalafil is the only drug of this class approved by the FDA for the treatment of lower urinary tract symptoms, though other agents have demonstrated similar efficacy.
Dual therapy with a PDE5 inhibitor and an alpha-blocker has greater efficacy than either monotherapy alone; however, caution must be exercised as these agents are titrated to avoid symptomatic hypotension. Lower urinary tract symptoms and sexual dysfunction often coexist; PDE5 inhibitors are appropriate in the management of such cases.
Even with effective medical therapy, the disease will progress in some men. In the MTOPS trial, the four-year incidence of disease progression was 10 percent for men on alpha-blocker or 5-alpha reductase inhibitor monotherapy and 5 percent for men on combination therapy. Between 1 and 3 percent of those in the various treatment groups needed surgery.
A number of effective surgical therapies are available for men with BPH, providing excellent one-year outcomes including a mean 70 percent reduction in IPSS and a mean 12 mL/sec improvement in peak urinary flow. With this in mind, patients whose symptoms do not improve with medical therapy, whose symptoms progress or who simply are interested in surgery should be referred for urologic evaluation.
Full references for this article are included in the unabridged version in the Cleveland Clinic Journal of Medicine. Dr. Unnikrishnan is a former urology resident now practicing in Virginia.
Advertisement
Pediatric urologists lead quality improvement initiative, author systemwide guideline
Fixed-dose single-pill combinations and future therapies
Reproductive urologists publish a contemporary review to guide practice
Two recent cases show favorable pain and cosmesis outcomes
Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood
Proteinuria reduction remains the most important treatment target.
IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy
Oncologic and functional outcomes are promising, but selection is key