Rates similar for both methods
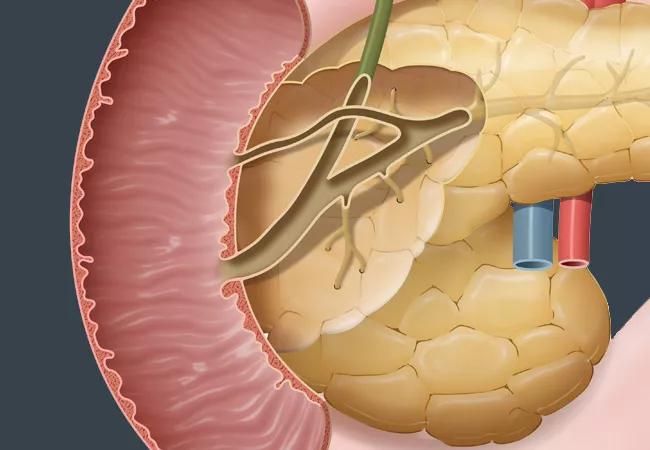
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/64379cf8-bb41-4fd3-8608-f9136dba65f0/21-DDI-2103514-CQD-Benign-Sporadic-Adenomas-DDW-2_jpg)
21-DDI-2103514-CQD-Benign-Sporadic-Adenomas-DDW-2
Recurrence rates for benign sporadic adenomas did not differ when treated with endoscopic vs. surgical ampullectomy, according to a systematic review and meta-analysis of 27 studies. Researchers from the Cleveland Clinic Digestive Disease & Surgery Institute’s Center for Advanced Endoscopy presented the findings of this review at Digestive Disease Week 2021.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Benign sporadic ampullary adenomas occur in patients without an adenomatous polyposis syndrome and have the potential to become ampullary carcinomas. For this reason, excision remains best practice. Endoscopic approaches are the most commonly used, with surgical approaches deemed appropriate for larger lesions, lesions with early cancer or adenomas extending inside the bile or pancreatic duct.
“The trend, where expertise is available, is toward more endoscopic ampullectomies, and we do have good data on the clinical outcomes of this approach,” says advanced endoscopist Prabhleen Chahal, MD, Program Director of the Advanced Endoscopy Fellowship in the Department of Gastroenterology at Cleveland Clinic, “but we don’t have long-term data on whether method of excision has an impact on recurrence.”
To fill this void in the literature, the research team, including Rajat Garg, MD, incoming gastroenterology fellow at Cleveland Clinic, conducted a comprehensive literature search using Cochrane, PubMed, Google scholar and Medline databases to identify any studies of endoscopic or surgical excision of sporadic ampullary adenomas that reported outcomes.
The final analysis included a total of 27 studies with 1,064 patients (741 endoscopic, 323 surgical), with a median patient age of 64 in the endoscopic group and 62.6 in the surgical group. The one-year pooled recurrence rate for endoscopic ampullectomy was 16.2 (95%, confidence interval [CI], 12.7-20.4, I2=19.6) versus 12.3 for surgical cases (95% CI, 8.5-17.4, I2 = 0.6, P = 0.2). At two years, the rate was 16.48 for endoscopic (95% CI, 11.28,-23.43, I2 = 40.6%), compared with 12.8 (95% CI, 8.42-18.98, I2=9.8%, P = 0.36).
Advertisement
The recurrence rate after three years was 18.89 for endoscopic procedures (95% CI, 12.89-26.83, I2=13.5%) versus 11.58 for surgical procedures (95% CI, 7.48-17.49, I2=5.5%) but was not statistically significant (P = 0.08). Only one study reported five-year recurrence rates for surgical ampullectomy, so a five-year comparison could not be established. Patient sex, age and size of lesion were not significant predictors of recurrence at any time interval.
“The study shows that, early on, there isn’t really a difference, but recurrence started trending up with endoscopic procedures at three years,” says Dr. Chahal. “That trend didn’t reach statistical significance, but the data simply doesn’t exist to determine whether that trend continues and does eventually become significant.” At Cleveland Clinic, a multidisciplinary team including a pancreatic surgeon reviews all patients who need ampullectomy before proceeding with endoscopic or surgical removal.
Advertisement
Advertisement
Benefits of neoadjuvant immunotherapy reflect emerging standard of care
Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence
Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors
Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling
Potentially cost-effective addition to standard GERD management in post-transplant patients
Findings could help clinicians make more informed decisions about medication recommendations
Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care
Retrospective analysis looks at data from more than 5000 patients across 40 years