Helps patients who aren't good surgical candidates
A cutting-edge endoscopy procedure that helps patients with gastric outlet obstruction is now available at Cleveland Clinic.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Endoscopic ultrasound-guided gastrojejunostomy (EUS-GJ) is a procedure in which physicians use an endoscope equipped with an ultrasound, camera, and electrocautery-enhanced lumen-apposing, self-expanding metal stent to create an anastomosis between the stomach wall and part of the small bowel loop beyond the area of blockage. This allows food to bypass the blockage and once again pass through the stomach and into the intestines.
Historically this bypass procedure has been performed through an open surgery on patients, which requires a hospital stay for recovery and is associated with possibility of complications related to surgery. Whereas, EUS-GJ has minimal to no such after-effects.
“It can be done as an outpatient procedure,” says Cleveland Clinic advanced endoscopist Prabhleen Chahal, MD. “There’s no recovery period involved and, even though there are no head-to-head trials comparing this innovative endoscopic technique to surgical bypass, the success and safety profile of EUS-GJ is highly promising.”
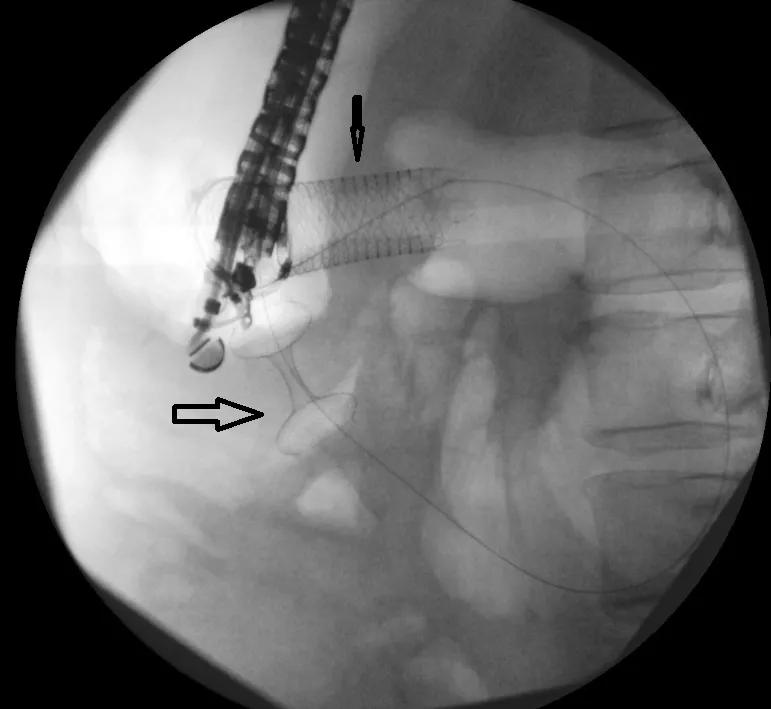
Dr. Chahal recently performed Cleveland Clinic’s first EUS-GJ on a patient with malignant gastric cancer whose tumor blocked a section of the duodenum. The patient had had a metal mesh duodenal stent endoscopically placed in the blockage to open it up, however, the tumor continued to grow and eventually plugged the stent.
To perform the EUS-GJ, Dr. Chahal and colleagues first anesthetized the patient and then inserted the endoscope into the patient’s mouth, passing through the stomach and into the small bowel. The camera on the instrument helped her assess the location and length of the blockage and helped her locate a section of the small bowel loop that was closest to the stomach but beyond the blockage. Finally, using ultrasound guidance, she used the cautery to puncture an opening in the stomach and small bowel loop and deployed a 2-cm long stent with flared ends (dumbbell shaped), which joined together the stomach and small bowel loop, creating an anastomosis.
Advertisement
Dr. Chahal says EUS-GJ is performed as a palliative measure for cancer patients who have a tumor that is creating the blockage and also for patients who are not good candidates for surgery. The bypass allows such patients to be able to continue to eat even as their disease progresses. It can also be performed on patients who have chronic diseases that can lead to blockages or strictures such as chronic pancreatitis.
She said the procedure is best for patient with blockages that appear in duodenum and is not appropriate for patients with a mid-small bowl blockage. It would also not work for patients with Crohn’s disease who tend to develop multiple blockages in several areas at the same time.
“We are hoping to raise awareness of this technique,” Dr. Chahal says. “It’s not for everybody, but for patients with a blockage in the stomach or early small intestine, it is an important option to consider.”
Advertisement
Advertisement

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years

Surgical intervention linked to increased lifespan and reduced complications