Shorter length of stay, fewer surgical site infections versus laparotomy
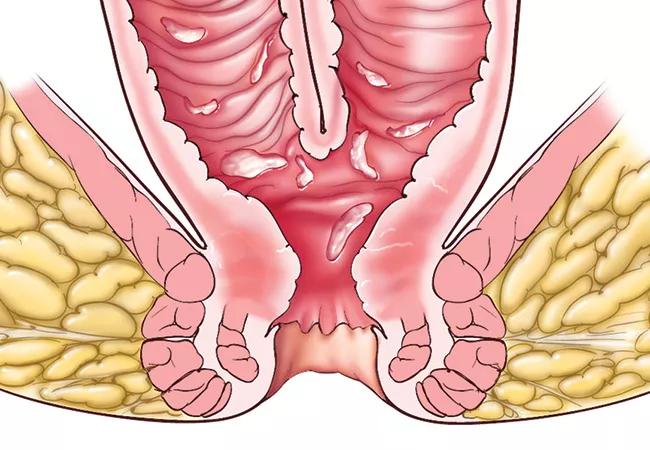
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f7cb611d-3ae3-4c30-a361-fe961a81df95/18-DDI-161-Ileal-Pouch-Feat_jpg)
18-DDI-161-Ileal-Pouch-Feat
Laparoscopic reoperative ileal J pouch anal anastomosis (IPAA) is feasible, safe and has better outcomes than laparotomy, according to a retrospective analysis of a Cleveland Clinic prospective database recently published in Surgical Endoscopy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Patients who undergo restorative proctocolectomy with IPAA for mucosal ulcerative colitis (MUC), Familial Adenomatous Polyposis (FAP) or other reasons, sometimes require pouch revision, advancement or excision, typically performed as laparotomy in a small number of referral centers. Up to 60% of patients will experience long-term complications that can be indications for IPAA reoperation, and 10 to 20% of patients will undergo a reoperative procedure. Reoperative surgery is very challenging due to scar tissue, the need to assiduously protect the blood supply to the J pouch, and limitations in the length of the mesentery restricting pouch mobility.
“These are technically complicated procedures, and we have not had adequate data about feasibility, safety and outcomes when performing them laparoscopically,” says Steven Wexner, MD, PhD, senior author of the study, Director of the Digestive Disease Center and Chairman of Colorectal Surgery at Cleveland Clinic Florida. “As a high-volume referral center, we perform among the highest volumes of these procedures; accordingly we wanted to add our experience to the literature.”
Researchers included all patients with MUC or FAP who underwent transabdominal reoperative IPAA surgery from 2011 to 2018 and excluded those who underwent primary IPAA, whose reoperative surgery was transperineal and who had pouches but non-pouch-related surgical indications.
Reoperation types were classified as pouch excision, pouch revision or pouch advancement. Pouch excision included abdominoperineal excision of the pouch and creation of end ileostomy. Pouch revision included transabdominal mobilization of the pouch, resection of part of a pouch or creation of a new pouch with re-anastomosis and creation of a diverting loop ileostomy. Pouch advancement included abdominoperineal mobilization of the pouch, reanastomosis and creation of diverting loop ileostomy. All patients had transabdominal pelvic drains placed and removed prior to discharge as well as ileostomy prior to or created during reoperation.
Advertisement
Nineteen of the 76 patients who met inclusion criteria underwent laparoscopic reoperative IPAA surgery, with 12 of those patients successfully treated laparoscopically and seven advancing to laparotomy, for an overall 63% intent to treat success rate. Patients who underwent laparoscopic surgery had significantly shorter length of stay (LOS) (5.5 vs. 9.7 days, P < 0.001) and significantly fewer abdominal superficial surgical site infections (SSI) (0% vs. 18%, P < 0.001) and deep SSI (0% vs. 17%, P < 0.001). No significant differences were found in overall complications, reoperation, readmission or mortality.
“Only the most experienced, high-volume laparoscopic IPAA surgeons should consider this approach,” says Dr. Wexner. “We found in this study that over time, our laparoscopic reoperations increased, and the success rate was directly dependent on the experience of the surgeon.”
While other studies have demonstrated the safety and feasibility of laparoscopic IPAA reoperation, this is the first to compare it directly to laparotomy. “While further study is needed,” notes Dr. Wexner, “this study shows clear benefit to reoperative transabdominal laparoscopic IPAA that should prompt further investigation and encourage referral to high volume centers for patients with MUC or FAP who may benefit from this approach.”
Advertisement
Advertisement
Benefits of neoadjuvant immunotherapy reflect emerging standard of care
Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence
Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors
Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling
Potentially cost-effective addition to standard GERD management in post-transplant patients
Findings could help clinicians make more informed decisions about medication recommendations
Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care
Retrospective analysis looks at data from more than 5000 patients across 40 years