Use of tool can change recommendation to add or omit radiation
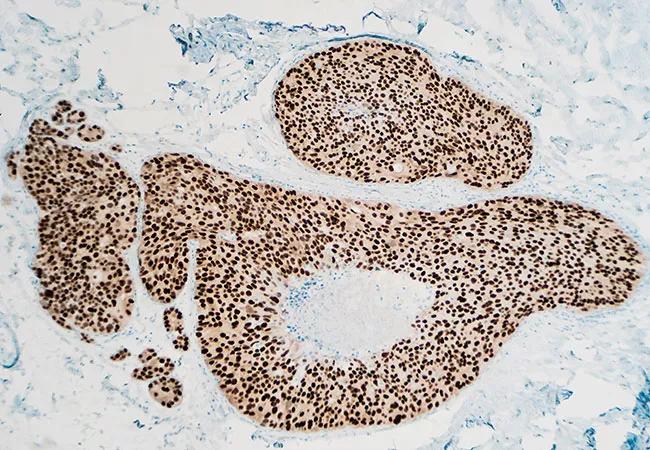
Incorporating a seven-gene assay with a novel biosignature (DCISionRT) is superior to clinicopathologic risk assessment alone in estimating the ten-year risk of recurrence for patients with ductal carcinoma in situ (DCIS) following breast conserving surgery as well as predicting benefit from radiation therapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“The risk of recurrence in patients with low-risk DCIS is 10 to 20% at 10 to 15 years post lumpectomy without radiation therapy,” says Chirag Shah, MD, Director of Breast Radiation Oncology and Director of Clinical Research-Radiation Oncology at Cleveland Clinic. “We traditionally use factors such as patient age, tumor size, margin status and tumor grade to define that risk. The problem we run into is that patients who are considered as having low recurrence risk, based on factors such as low-grade disease, smaller tumor size and negative margins, still have elevated rates of recurrence when radiation is omitted. In studies comparing radiation and no radiation, even these low-risk patients derive a benefit from radiation, which informs us that we haven’t been able to pick out the group that does not benefit from radiation using traditional clinicopathologic features.”
In contrast, the biosignature combines biomarkers and four clinicopathologic factors to assess individual tumor biology, providing a personalized recurrence risk. In the analysis, 926 women from four cohorts who were treated with BCS with negative margins, with or without adjuvant radiation, had a decision score calculated using DCISionRT. Based on their score, patients were classified as either low risk, elevated risk or residual risk. Dr. Shah presented the findings at the 2022 American Society for Radiation Oncology meeting.
The low-risk group, approximately 37% of all patients, were found not to derive a benefit from adjuvant radiation with respect to ten-year recurrence rates. The elevated-risk group, which represented about 43% of patients, experienced a significant benefit from radiation therapy, with the risk of recurrence declining from 21% to about 5% with the addition of radiation therapy, corresponding to an 80% reduction in risk (P<0.001). The benefit persisted even in those patients with good clinicopathologic features who were to have elevated risk DCISionRT scores.
Advertisement
“The final group, the 20% of patients with residual risk, were found to benefit from adjuvant radiation (42% vs. 15%) but still had elevated rates of recurrence even after treatment. This was a major finding of the study,” says Dr. Shah. “There are some patients we treat with all standard treatment and yet they still have a recurrence. We have to figure out who these patients are. The residual risk group makes up a small percentage of the total number of patients, but they had almost a 15% rate of recurrence even after lumpectomy and radiation, compared with 5% in the other groups, a three-fold higher risk.”
Additionally, Dr. Shah and colleagues previously found that the information provided by DCISionRT often changed recommendations to add or omit radiation therapy following breast-conserving surgery in patients with DCIS—approximately of 40% patients had a change in radiation therapy recommendation (46% from recommending radiation therapy to omitting radiation, and 35% from omitting to adding radiation).
DCISionRT is offered in clinical practice at Cleveland Clinic, where research on its clinical utility continues.
Advertisement
Advertisement

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Reconsidering axillary lymph node dissection as well as depth of surgical margins

Ultra-Hypofractionated Whole Breast Irradiation and Partial Breast Irradiation Reduce Many Toxicities

Best practices for reducing toxicities

Partnerships with local social service agencies key to program success

Ongoing clinical validation refine breast cancer risk substratification

Phase 3 trial found no survival differences between weekly or biweekly doxorubicin/cyclophosphamide or between weekly or biweekly paclitaxel

Findings strengthen evidence for risk-reducing procedures