Tumor genomics offer clues for identifying high risk of relapse
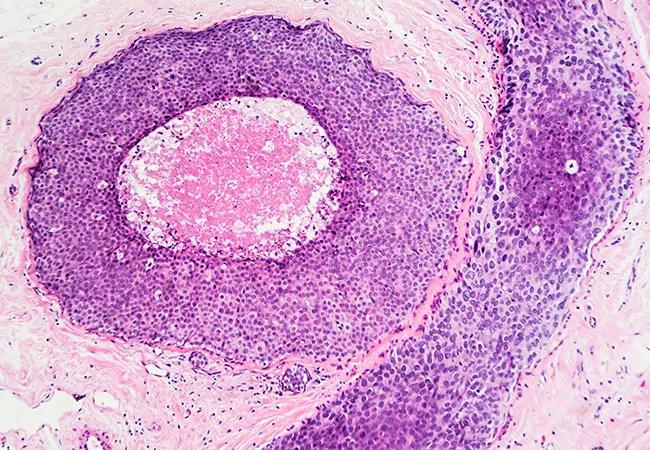
Until recently, there was little way to discern which patients diagnosed with ductal carcinoma in situ (DCIS) had a low recurrence risk and could forgo radiation therapy after breast conserving surgery and who needed more aggressive treatment. By evaluating tumor biology and genomics, researchers have found that they can now use these tools for risk stratification to better determine the adjuvant treatments needed for each patient.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Last year at the American Society for Radiation Oncology (ASTRO) annual meeting, researchers presented findings of a multi-institutional study using a biosignature called DCSionRT® to classify patients into two different risk categories: Low-risk patients who derived minimal benefit from adjuvant radiation and elevated risk patients who benefited from radiation therapy.
Building on this research, the team has since discovered that a subset of the high-risk patients fit into a poor response category. These patients face a high recurrence rate, despite undergoing lumpectomy and radiation.
“Traditionally, pathology reports and clinicopathologic data were used to identify the appropriate treatment strategy for each patient with DCIS, but we’ve seen from clinical trials that this is not particularly effective in identifying low-risk patients,” says Chirag Shah, MD, study co-author and director of Breast Radiation Oncology at Cleveland Clinic. “With new prognostic tools, we will be able to offer patients who are lower risk the comfort of potentially skipping radiation and those with an elevated risk the confidence that going forward with radiation or other treatments is necessary.”
Pathology, clinical data and formalin-fixed paraffin-embedded tissue (FFPE) samples were evaluated for 485 women treated for DCIS with lumpectomy with negative margins, with or without whole breast radiation therapy, at centers in Sweden, the U.S. and Australia. The study also assessed a subset of patients with large tumor size (>2.5 cm) and/or nuclear-grade III DCIS. A validated biosignature (Prelude, Laguna Hills CA) and a novel response subtype biosignature to radiation therapy after lumpectomy were determined using protein biomarkers (p16/INK4A, Ki-67, COX-2, PgR, HER2, FOXA1, SIAH2) assayed on FFPE tissue.
Advertisement
The two biosignatures classified patients into three risk groups: Low risk, elevated risk with a good response subtype and elevated risk with a poor response subtype. Ipsilateral breast tumor recurrence (IBTR) included DCIS or invasive breast cancer (IBC) that was local, regional or metastatic. Hazard ratios and 10-year risks were calculated using Cox proportional hazards and Kaplan-Meier analyses.
Of the 250 patients with nuclear grade III DCIS and/or size >2.5 cm, the biosignatures classified 72% (n=179) of patients into an elevated risk group consisting of those with a good (n=122) or a poor (n=57) response subtype to radiation therapy after lumpectomy. The remaining 28% of patients were classified into a low-risk group (n=71). In the low-risk group (n=71), patients treated without radiation therapy had good 10-year outcomes with no (0%) 10-year IBC events, and derived no significant radiation therapy benefit (1%) in 10-year IBTR rates (IBTR p=0.81).
Of all patients treated without radiation therapy (n=102), those in the elevated risk group (good and poor response subtype combined, n=61) had significantly worse 10-year IBTR/IBC rates (31%/17%) than those in the low-risk group, (IBTR HR=12, p=0.01). Patients treated with radiation therapy in the elevated risk group with a good response subtype (n=77) had significantly reduced 10-year IBTR/IBC rates of 5%/3%. However, no significant benefit to radiation therapy was noted for patients within the elevated risk group with a poor response subtype (n=41), who had 10-year IBTR/IBC rates of 25%/20%. Of all patients treated with radiation therapy in the elevated risk group (n=118), those with a poor response subtype had significantly worse outcomes than those with a good response subtype (IBTR HR=4.1, p=0.035, IBC HR=8, p=0.053).
Advertisement
Dr. Shah predicts that based on these findings, there will soon be three approaches for DCIS treatment following lumpectomy:
Studies show that overall, the rates of mortality associated with breast cancer are very low with DCIS, yet there is a subset of patients who are at higher risk of mortality. A recent 10-year retrospective randomized study in Sweden was consistent with these findings. The goal is to identify those patients in order for clinicians to optimize their therapies and reduce that risk. “The aim is to limit overtreatment of patients for whom a lumpectomy is enough and just importantly, to make sure we don’t undertreat those with a higher probability of this risk,” says Dr. Shah.
In a follow-on study, Dr. Shah led a team of researchers to analyze the impact of DCISionRT on clinicians’ recommendations for radiation therapy. The findings showed that use of DCISionRT led to a substantial overall change (42%) in the radiation recommendation, resulting in a 20% absolute net decrease in radiation therapy recommendation. Additionally, post-test radiation therapy was recommended to 35% of patients who had not previously received this recommendation. The results demonstrated the utility of this prognostic tool in routine practice for making radiation therapy decisions.
Advertisement
As genomic testing becomes more emergent in clinical practice, researchers will continue to follow patients to understand how testing is impacting both recommendations about radiation therapy and subsequent outcomes.
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient