How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program

Podcast content: This podcast is available to listen to online.
Listen to podcast online (https://www.buzzsprout.com/2250706/17432497)
From its inception in 2016 through its expansion during the COVID-19 pandemic to where it is today, Cleveland Clinic’s Point-of-Care Ultrasound (POCUS) program has become a model for integrating POCUS into clinical practice.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In a recent podcast episode of Respiratory Exchange, Abhijit Duggal, MD, speaks with Siddharth Dugar, MD, and Ajit Moghekar, MD, MBA, two critical care medicine specialists who were involved with the development and expansion of Cleveland Clinic’s POCUS program.
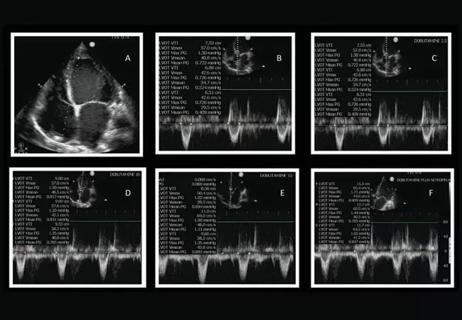
Today, over 1,400 cardiac ultrasounds, 600 lung ultrasounds, and more than 2,000 vascular ultrasounds are performed annually, with a median time of 5.5 hours from ICU admission to ultrasound completion, emphasizing rapid diagnostic support.
Dr. Moghekar recounts that when he first came to Cleveland Clinic in 2011, there was an ultrasound machine for the 64-bed medical ICU. One of his priorities was to establish and develop a POCUS program. By 2016, Dr. Dugar was named director of POCUS, and they have since increased from one ultrasound machine to 15 in the ICU. The COVID-19 pandemic accelerated the program’s development even further.
“Because we had such a robust program already in place by that point and to reduce exposure to all our radiology and cardiology colleagues, we took over performing the whole-body ultrasound,” says Dr. Moghekar. “…what we were able to do was on day one, was that as soon as a patient came to the ICU, we performed ultrasound exam in the heart, the lung and the venous system to make sure that the treatment that is provided to our patients did not get compromised, while also reducing the exposure to healthcare providers.”
In addition to discussing the program’s development and growth, Drs. Duggal, Dugar and Moghekar also touch on:
Advertisement
Click the podcast player above to listen to the episode now, or read on for a short, edited excerpt. Check out more Respiratory Exchange episodes at clevelandclinic.org/podcasts/respiratory-exchange or wherever you get your podcasts.
Dr. Duggal: We are seeing a lot that has changed in the last decade or so. Tell me a little bit about where ultrasonography and critically ill patients are going. With all the technological advances that we are seeing, where do you both see this technology going over the next few years, Dr. Dugar?
Dr. Dugar: Well, I think the best analogy that comes to my mind is the digital single-lens reflex (DSLR) camera and the point-and-shoot camera. Right now, ultrasound is at the DSLR phase, so it's very training-dependent. You have to make sure you change your aperture, you make sure that the light is good, but with the integration of AI and a lot of software coming out, I'm pretty sure that, not too far in the future, we will be seeing where you just basically put an ultrasound on the patient. It will be able to optimize and acquire the best image possible, and also interpret the images for you. Your job at this will be to make sure that the interpretation is accurate and how best to apply that information provided to your patient care.
Another thing, as Dr. Moghekar previously mentioned, was miniaturization of the chip. As chips are getting smaller and smaller, we are getting ultrasound data that is also smaller. We are not far away from having ultrasound stickers being placed on the patient that can provide a continuous assessment of a vessel, of the cardiac function, or just being placed in the heart will give us accurate pressure monitoring so we can be very precise when it comes to management of our patients.
Advertisement
Dr. Duggal: Thank you so much. Dr. Moghekar?
Dr. Moghekar: If I can add to that analogy, I think the ultrasound is in the stethoscope stage. Medical schools are heavily investing in teaching our medical students how to use ultrasound right from the first year. There are some medical schools that hand out point-of-care ultrasounds to medical students. So, I think point-of-care ultrasound is here to stay. It is going to be used to be able to see a lot of applications, not only in the ICU, but outside the ICU as well. With the help of artificial intelligence and technology, I think it's going to be easy.
I can easily see a day where patients have ultrasounds with them at home and they're monitoring their own health using a point-of-care ultrasound, and we as physicians are just looking at those images and giving them guidance. I think the one area where I think point-of-care ultrasound can improve is in regard to resources — areas where medical facilities are not available. Point-of-care ultrasound can fill the void there. So, I'm really excited to see how far we can take this field and artificial intelligence and smaller chips coming along. I think the sky is the limit.
Advertisement
Advertisement
A recent case illustrates how timely and appropriate use of POCUS can provide benefits at all stages of the care path

Nurse-led research provides surprising insights

Cleveland Clinic research emphasizes taking a holistic and individualized approach to care of septic shock

Historic collaboration connects two Cleveland Clinic locations, enables real-time sharing of metrics and surgical progress

AHA scientific statement outlines models for high-intensity staffing, specialized expertise and more

Consider this rapidly changing, cutting-edge specialty

Dynamic modeling improves the accuracy of outcome predictions for ICU patients

Fellow critical care nurses welcome additional support and expertise