A recent case illustrates how timely and appropriate use of POCUS can provide benefits at all stages of the care path
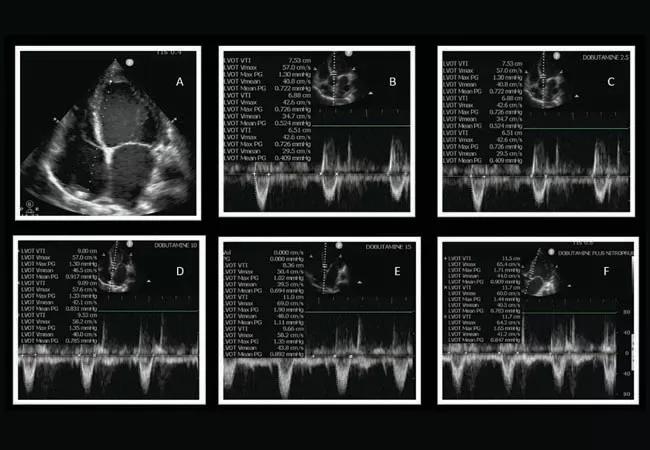
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8315e66d-0db7-48a6-a1d5-866c47720da6/22-PUL-3153138-CQD-Complex-Case-3-DrsDuggal-Dugar650x450_jpg)
POCUS
Figure A: The image shows a dilated left ventricle. Figures B – E: The images show increase in LVOT VTI (surrogate for stroke volume/cardiac output) with increase in dobutamine dosage from the 15 µg/kg/min shown in Figure E. Figure F: The image shows additional increase in LVOT VTI (surrogate for stroke volume/cardiac with addition of nitroprusside.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Written by Abhijit Duggal, MD, and Siddharth Dugar, MD
A 59-year-old with a history of bipolar disorder, HIV (recent CD4 score of 658 on
antiretroviral treatment [ART] therapy), cocaine abuse complicated by non-ischemic dilated cardiomyopathy and seizure disorder was admitted to our MICU from an outside hospital. The patient presented with concerns for respiratory failure and concern for medication-induced liver injury.
On arrival, the patient decompensated with worsening shock and encephalopathy,
which required mechanical ventilation. The workup for shock, encephalopathy and
liver injury included CT of the patient’s head, electroencephalogram (EEG), liver
imaging and culture, which all failed to show any pathology.
Over the following 24 hours, the patient’s hemodynamic status, mental status
and lactate levels improved with fluid resuscitation and antibiotics. Spontaneous
breathing trial attempts were associated with tachycardia, tachypnea and increased lactate levels. A chest X-ray was performed to determine the etiology of the patient’s spontaneous breathing trial (SBT) failure and showed minimal bibasilar infiltrates. A bedside (POCUS) cardiac assessment was performed, which showed severely dilated and severely reduced left ventricular cardiac function. The POCUS was also used as a hemodynamic monitoring device to measure stroke volume and cardiac output with validated pulse wave Doppler LVOT VTI technique. The cardiac output was found to be significantly reduced in comparison to the previous echocardiogram.
Advertisement
The patient’s failure to transition from the mechanical ventilator to spontaneous breathing was attributable to his compromised left ventricular systolic function. The patient was started on dobutamine, an inotropic agent to increase cardiac output. The medication was titrated using POCUS-guided cardiac output measurement.
Once it was observed that up-titration of dobutamine further increased cardiac output, nitroprusside was added. The optimal dosage of nitroprusside was again guided by trending the cardiac output, obtained using POCUS. Over the next 24 hours, the cardiac output was optimized using POCUS, and the patient was successfully extubated. Following the transition from intravenous medication to oral medication, the patient was discharged home.
POCUS is widely used as a diagnostic modality in critically ill patients. The application of POCUS as a hemodynamic monitoring device to guide management and tailor intervention requires expertise in both image acquisition and interpretation.
In the current case, timely use of POCUS determined the cause of weaning failure as the inability of the heart with impaired cardiac function to cope with the transition from positive-pressure ventilation to breathing without the ventilator. In addition, POCUS also guided the titration of medication, which routinely requires invasive monitoring devices including pulmonary artery catheter to facilitate weaning from the ventilator.
Timely and appropriate application of POCUS by an expert can hasten diagnosis, guide appropriate interventions and minimize the need for invasive hemodynamic monitoring.
Advertisement
Advertisement
How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program
Cleveland Clinic pioneers a new paradigm in cardiovascular care delivery
Site visits offer firsthand lessons in clinical and operational excellence in cardiovascular care
Historic collaboration connects two Cleveland Clinic locations, enables real-time sharing of metrics and surgical progress
Consider this rapidly changing, cutting-edge specialty
Oral medication reduces epistaxis and improves quality of life for patients with rare vascular disorder
Cancer drug helps treat decades-long symptoms in patient with complicated lymphatic issue
Cleveland Clinic study finds that durable weight loss is key to health benefits