A New Standard of Care in Relapsed/Refractory Large B-Cell Lymphoma
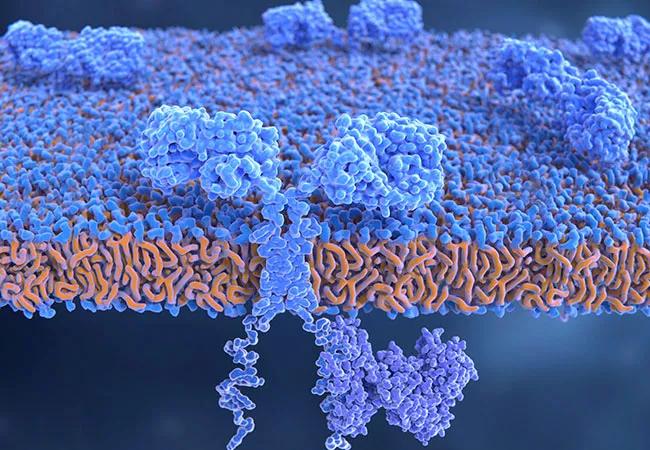
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/177a8b2b-6604-45b6-9eee-d8b04f4b2099/22-CNR-2889558-CQD-Hero-650x450-Yescarta_jpg)
22-CNR-2889558-CQD-Hero-650×450 Yescarta
Patients with large B-cell lymphoma who relapse on first-line chemoimmunotherapy typically have a poor prognosis. Until recently, the standard second-line treatment for these patients consisted of high-dose chemotherapy coupled with autologous stem cell transplantation in those patients who respond to chemotherapy. However, the outlook for this difficult-to-treat population of lymphoma patients has changed with the updated FDA approval of axicabtagene ciloleucel (axi-cel; YESCARTA®) on April 1, 2022.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“As many as 30% of patients with large B-cell lymphoma will not respond to or will relapse after front-line treatment,” says Brian Hill, MD, PhD, Director of the Lymphoid Malignancies Program and a staff physician in the Cleveland Clinic Taussig Cancer Institute. “Historically, somewhere around 40% of those patients with relapsed/refractory large B-cell lymphoma are cured with an autologous stem cell transplant, but over half of patients never make it to transplant because their disease does not respond sufficiently well to make the high-dose chemotherapy worthwhile as part of the transplant maneuver.”
Axi-cel, an autologous anti-CD19 chimeric antigen receptor (CAR) T-cell therapy, was initially approved in 2017 for adult patients with large B-cell lymphoma but it was reserved for patients who had already undergone autologous stem cell transplant or were unable to receive such treatment. The updated FDA approval is a formal indication for patients who have lymphoma that is refractory to first-line chemoimmunotherapy or for those who relapsed within 12 months of first-line chemoimmunotherapy. The approval was based on the results from ZUMA-7, a multicenter Phase 3 trial that compared the efficacy of axi-cel to standard care chemoimmunotherapy followed by high-dose chemotherapy with autologous stem cell transplantation in patients with relapsed or refractory large B-cell lymphoma.
According to Dr. Hill, who served as the lead for the Cleveland Clinic arm of the trial, the motivation behind ZUMA-7 was the need to develop novel therapies for those patients whose disease does not respond to salvage chemotherapy and therefore could not be transplanted, or for those who relapse after transplant.
Advertisement
“We know that CAR T-cell therapy worked better than anything else previously studied in that setting,” he says. “In fact, somewhere around 40% of the patients who get CAR T-cells after auto transplant or who are ineligible for transplant can probably be cured with CAR T-cell treatment. The reasoning for the study was to compare what the standard of care was versus CAR T-cell therapy.”
ZUMA-7 randomized a total of 180 patients to receive axi-cel and 179 to receive the standard of care. Event-free survival served as the primary endpoint. At a median follow-up of 24.9 months, the median event-free survival was 8.3 months and 2.0 months in the two respective groups, and the 24-month event-free survival was 41% and 16%, respectively. 83% of patients treated with axi-cel and 50% of those treated with the standard of care achieved a response. At two years, the estimated overall survival was 61% in the axi-cel arm and 52% in the standard-of-care arm.
“The CAR T-cell treatment did perform better as measured by event-free survival, and there was a trend towards an improvement in overall survival from the time of being registered on the study,” Dr. Hill says.
In terms of the side effect profile, significant toxicities were observed with both treatments.
“The overall period of hospitalization with autologous stem cell transplant is typically longer than with CAR T-cell therapy, but CAR T-cell therapy does have some unique toxicities, including cytokine release syndrome (CRS) and neurologic toxicities,” he says. “These are largely reversible, but still can be difficult for older or frailer patients with comorbidities in particular to safely go through.”
Advertisement
Dr. Hill believes the findings of the ZUMA-7 trial represent a significant improvement in the standard of care for large B-cell lymphoma in the second-line setting.
“This is a major breakthrough for patients with this difficult-to-treat lymphoma. Although it may be difficult for some [patients] to undergo CAR T-cell treatment at the current time, we anticipate that in the future, newer cell therapies and other strategies will likely become available to allow this approach to be offered to a wider range of patients,” he says. “Axi-cel allows patients to avoid transplants and also may allow for longer survival on average, although I think we need a little more data or follow-up to see over the long term what happens with survival.”
In addition to axi-cel, there is much momentum occurring in the CAR T-cell therapy field for treating lymphoma. In June, the FDA also approved lisocabtagene maraleucel (Breyanzi®), a CD19-directed CAR T-cell therapy for relapsed/refractory large B-cell lymphoma.
Advertisement
Advertisement
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality