Restorative procedures produce better outcomes and durability
By Paul Saluan, MD, and David Zhu, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cartilage injuries are a common cause of pain in children and young adults. These injuries, most commonly in the knee, can be traumatic, such as through a direct impact or dislocation, or from repeated microtrauma arising from instability or pathologic biomechanics. It is essential to identify and treat these lesions, not only to relieve pain and restore function, but also to prevent the earlier development of osteoarthritis.
In evaluation of these patients, in addition to a standard knee examination — gait, range of motion, effusion, crepitus and palpation — it is important to assess the body habitus and alignment (including with full-length lower extremity radiographs), as they may be underlying mechanical contributors to the disease process (Figure 1). In addition to radiographs, MRI is essential for identification, sizing and characterization, as well as for assessment of the subchondral bone for fractures (Figure 2). Since the focal lesion is typically surrounded by degenerative or poor-quality cartilage (Figure 3), MRI actually underestimates the area required for debridement by up to 65%.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8d2ecb85-d0ba-46e0-bc47-d419c277e22c/21-ORI-2429062-Inset-1-755x1024_jpg)
Figure 1. Full-length lower extremity radiograph showing normal alignment, with the mechanical axis passing through the center of the knee.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/271edee8-619f-41fb-8c73-614df5930d91/21-ORI-2429062-Inset-2_jpg)
Figure 2. MRI showing cartilage lesion with associated subchondral edema.
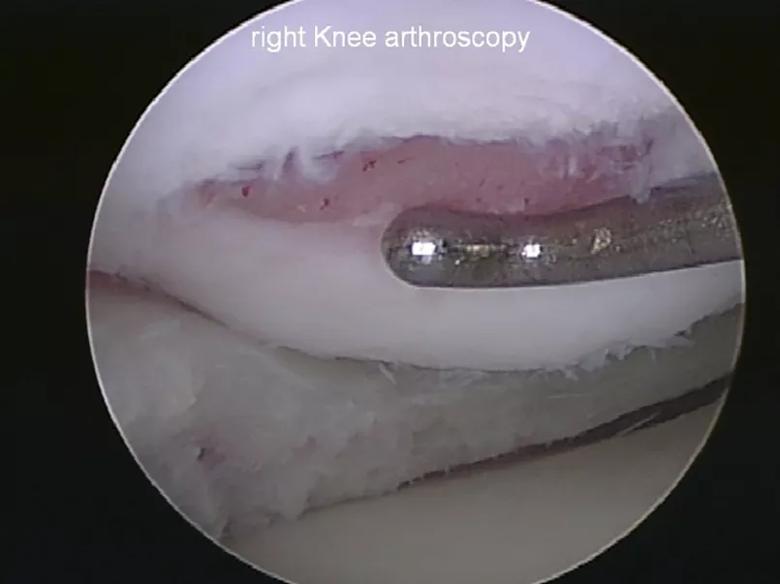
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/19f1ac4e-40ea-4bce-86e1-7d53ea12e063/21-ORI-2429062-Inset-3_jpg)
Figure 3. Arthroscopic view of a cartilage lesion of the femoral condyle.
Initial treatment for cartilage injuries consists of activity modification, NSAIDs, bracing, physical therapy, and corticosteroid or viscosupplementation injections, but it is important to note that these interventions are only for symptom modification and do not address the underlying pathology. Patients failing conservative management, or who have mechanical symptoms, loose bodies, recurrent effusions or focal lesions, are indicated for surgery. Surgery must also address any ligament deficiency or malalignment present in order to optimize biomechanical conditions for healing and survival of chondrocytes.
Advertisement
As cartilage cannot regenerate, surgical options are either reparative or restorative. Reparative marrow-stimulation procedures, such as microfracture, introduce undifferentiated mesenchymal cells into the lesion and fill the lesion with mechanically inferior fibrocartilage. Longer-term studies suggest microfracture may not be durable over time. Because these procedures involve an intra-articular inflammatory phase, they also lead to increased failure rates for subsequent cartilage procedures.
Restorative procedures, such as those involving cartilage allografts, matrix-associated autologous chondrocyte implantation (MACI) and osteochondral autograft transplantation (OAT), attempt to reintroduce hyaline cartilage into the lesion. Restorative options are based on the size and location of lesion, with smaller lesions generally favoring treatment with cartilage allograft or OAT, and larger lesions requiring treatment with MACI or size-matched bulk grafts.
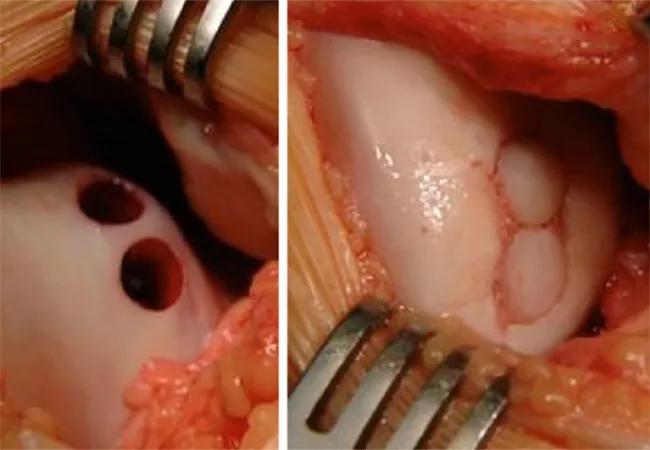
Several types of cartilage allografts are commercially available. BioCartilage® (Arthrex, Inc.) is a putty containing cartilage extracellular matrix that can be used to fill defects. DeNovo® NT Graft (Zimmer Biomet) is a particulated juvenile cartilage graft that also can be used to fill defects. Cartiform® (Osiris Therapeutics, Inc.) is a sheet of allograft cartilage that is matched to the size of the lesion and then fixed in place in the defect using anchors and suture (Figure 4).
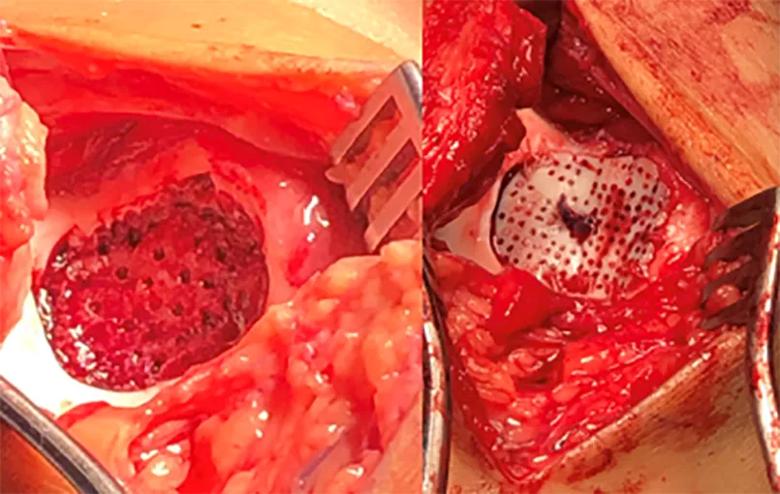
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f1f32ce3-8721-49ac-baef-25a4805a9de8/21-ORI-2429062-Inset-4_jpg)
Figure 4. Cartiform procedure with implantation site on the trochlea.
Advertisement
MACI is an effective option for lesions that are larger or located in an area of the joint difficult to match with a graft, such as the patellar trochlea. It is a two-stage procedure. First, a biopsy of healthy cartilage is obtained arthroscopically either from a non-weight-bearing area of the joint or from an area of cartilage that would otherwise be debrided. The specimen is processed to extract and culture the chondrocytes. After about four weeks, a membrane containing the expanded chondrocytes is replanted into the lesion (Figure 5).
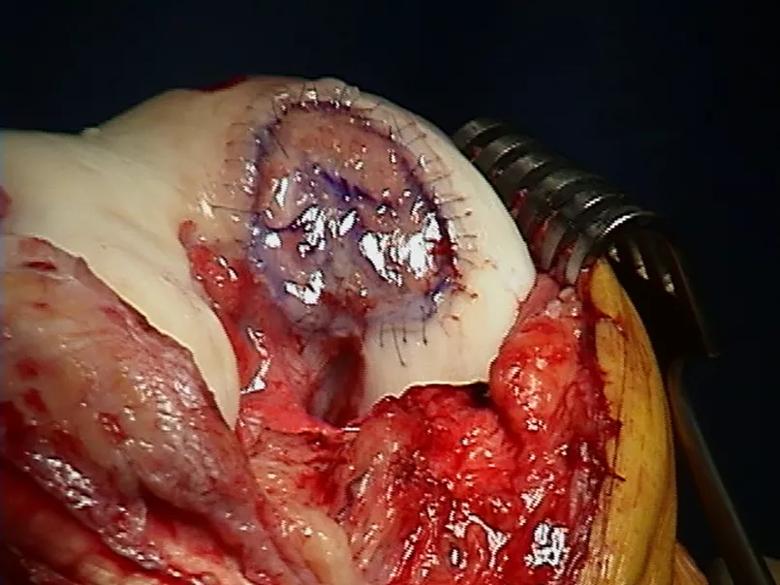
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ab88dbbf-85c8-452f-8371-5b0beee81b13/21-ORI-2429062-Inset-5_jpg)
Figure 5. MACI membrane filling cartilage lesion, affixed with suture and fibrin glue.
OAT procedures involve transferring plugs of cartilage along with underlying bone from a non-weight-bearing area of the joint (such as the intercondylar notch or medial side of the patellar trochlea) to the defect (Figure 6). This procedure fills the defect with native hyaline cartilage and also addresses subchondral bone problems. The osteochondral plugs also allow for direct bone-to-bone healing with the area surrounding the lesion.
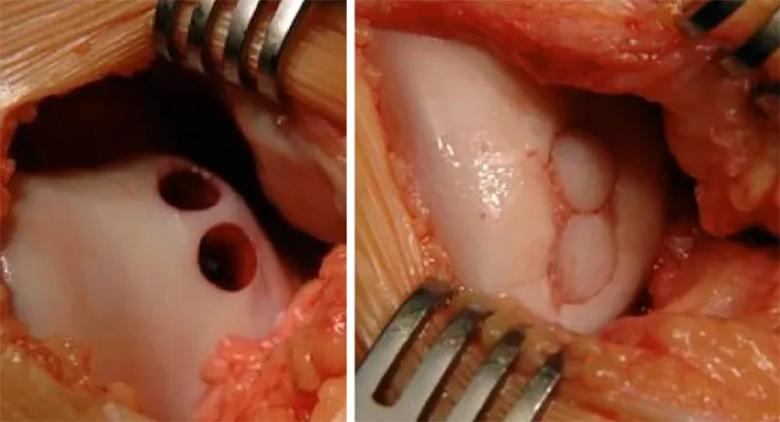
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8f5c0a6f-dcdf-4747-bcd0-f9dcbbbfa423/21-ORI-2429062-Inset-6_jpg)
Figure 6. OAT procedure showing the donor site on the medial trochlea and implantation site on the femoral condyle.
OAT is ideal for smaller lesions (< 2.5 cm2) in active patients with high physical demands. If mechanical malalignment is present, it should be corrected with a concurrent osteotomy.
Alternatively, a fresh allograft may be used as the source of the osteochondral plug. For smaller lesions, off-the-shelf osteochondral plugs are available. For larger lesions, bulk allografts matched by size and location to the lesion can be used. These grafts are processed to preserve the existing cartilage and chondrocytes but remove the cellular and immunogenic components of the bone and, therefore, do not require immunosuppression. Studies have shown a high rate of return to play in athletes after either autograft or allograft osteochondral transplant procedures.
Advertisement
Overall, treatment of cartilage lesions has transitioned from reparative to restorative procedures as cartilage grafts have shown to have improved outcomes and durability, and as a wider array of biologic graft options has become available. These options allow us to help children with these injuries reduce pain, improve function, return to physical activity and reduce the risk of developing osteoarthritis.
Dr. Saluan is Director of Pediatric and Adolescent Sports Medicine at Cleveland Clinic. Dr. Zhu is a fellow in orthopaedic sports surgery.
Advertisement
Advertisement

How it’s similar but different from the direct anterior approach

Collaboration must cross borders and disciplines

Systematic review of MOON cohorts demonstrates a need for sex-specific rehab protocols

Should surgeons forgo posterior and lateral approaches?

How chiropractors can reduce unnecessary imaging, lower costs and ease the burden on primary care clinicians

Why shifting away from delayed repairs in high-risk athletes could prevent long-term instability and improve outcomes

Multidisciplinary care can make arthroplasty a safe option even for patients with low ejection fraction

Percutaneous stabilization can increase mobility without disrupting cancer treatment