Innovative treatments control cancer recurrence
After yet another recurrence, a 69-year-old breast cancer patient sought a consultation at Cleveland Clinic in 2017. She was diagnosed in 2007 with Stage II (T1N1M0) ER-positive, PR-positive, HER2-negative right breast cancer and underwent a lumpectomy, adjuvant chemotherapy, radiation and adjuvant hormonal treatment (anastrozole). Following an in-breast recurrence in 2009, she had a mastectomy, and her hormonal treatment was changed to tamoxifen which she took until 2015 when she experienced a right chest wall recurrence. She had surgery again and her hormonal treatment was changed to fulvestrant. In 2016, she experienced additional nodules in the right chest wall, which was first monitored, then an excision was attempted in early 2017.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“When she started to experience further recurrences in the chest wall, things became more complicated and it made sense to have a multidisciplinary evaluation with a team experienced in dealing with recurrent breast cancer,” says Halle Moore, MD, Director of Breast Medical Oncology in the Department of Hematology and Oncology at Cleveland Clinic Cancer Center and Co-Director of the Cleveland Clinic Comprehensive Breast Cancer Program.
Dr. Moore arranged a consultation with radiation oncologist Chirag Shah, MD, who recommended reirradiation with hyperthermia to the right chest wall. Hyperthermia increases temperatures to make tumor cells more sensitive to radiation. By adding hyperthermia to radiation therapy, radiation oncologists can improve tumor control while minimizing damage to healthy tissue. Cleveland Clinic is one of only a few medical centers to offer this treatment.
“Hyperthermia is commonly used for breast cancer recurrences. Adding hyperthermia to radiation improves outcomes and has low rates of long-term side effects based on published studies,” says Dr. Shah. It also enables a lower dose for a second course of radiation. In one study of hyperthermia treatment for recurrent breast cancer, the response rate was 60 percent with hyperthermia compared with 38 percent without hyperthermia.
After the hyperthermia re-irradiation, the patient’s hormonal therapy was changed to exemestane. She has remained free of recurrence in that area.
While the patient’s right side was stable, during routine follow up in the fall of 2019, she was found to have large contralateral (left) axillary adenopathy with the biopsy detecting what appeared to be metastasis from her original cancer. No new disease was identified in the left breast. Fortunately, she had no other evidence of distant metastasis but did have fairly extensive involvement in the lymph nodes in the left axilla. She received chemotherapy with capecitabine and had an excellent response.
Advertisement
“Given this good response and that her metastatic disease was so limited, we again suggested an aggressive approach to try to gain long-term control,” says Dr. Moore.
Her medical team recommended an axillary lymph node dissection with lymphaticovenous bypass; this procedure was developed at Cleveland Clinic to protect against lymphedema through enhanced lymphatic visualization during axillary reverse mapping (ARM) and better decision-making during lymphaticovenous bypass. Following the surgery, she would have radiation to the left chest wall and regional lymph nodes including those in the axilla.
The patient was scheduled for the procedure in early April, which coincided with the first COVID-19 surge when many surgeries were being cancelled or delayed. While cancer surgeries are considered essential procedures and have been allowed to continue throughout the pandemic, the lymphaticovenous bypass could be considered elective and deferred to a later time. However, based on concerns about whether the procedure could be done after radiation, “the patient’s providers advocated for her and were able to proceed with what we felt was her best option for prevention of long-term complications from this multi-modality approach to her disease,” says Dr. Moore.
She also received further systemic therapy with letrozole and palbociclib, a CDK4/6 inhibitor.
Following treatment, the patient has been maintained on endocrine therapy plus palbociclib. At her last visit in September 2020, “she was doing very well with no evidence of active cancer and no concerns with lymphedema,” says Dr. Moore.
Advertisement
Dr. Moore attributes the successful outcome to multidisciplinary care: “Communication among medical oncology, radiation oncology, surgical oncology and plastic surgery really helped to develop the best plan for this patient. We figured out the timing of treatments, knowing how local treatment, surgery and radiation work together, and how plastic surgery can reduce morbidity. We not only achieved good control of her disease but also minimized long-term treatment effects.”
“Never hesitate to reach out to your colleagues to develop and coordinate care,” she says.
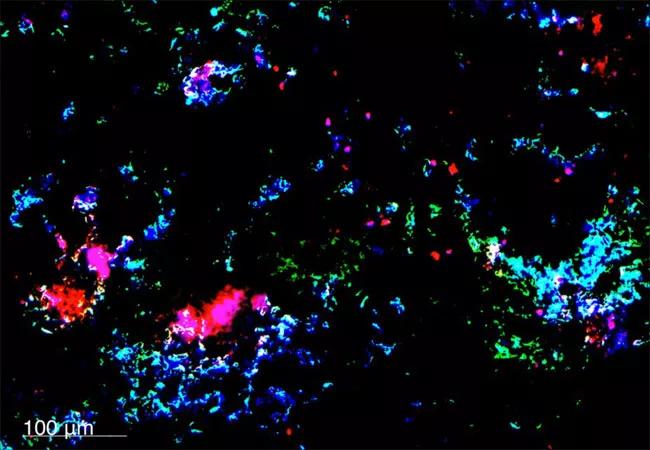
Image: Nanoparticles in breast cancer metastases. Image source: National Cancer Institute/Case Western Reserve University
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors