Patient with quadruple refractory multiple myeloma achieves complete response with cell therapy
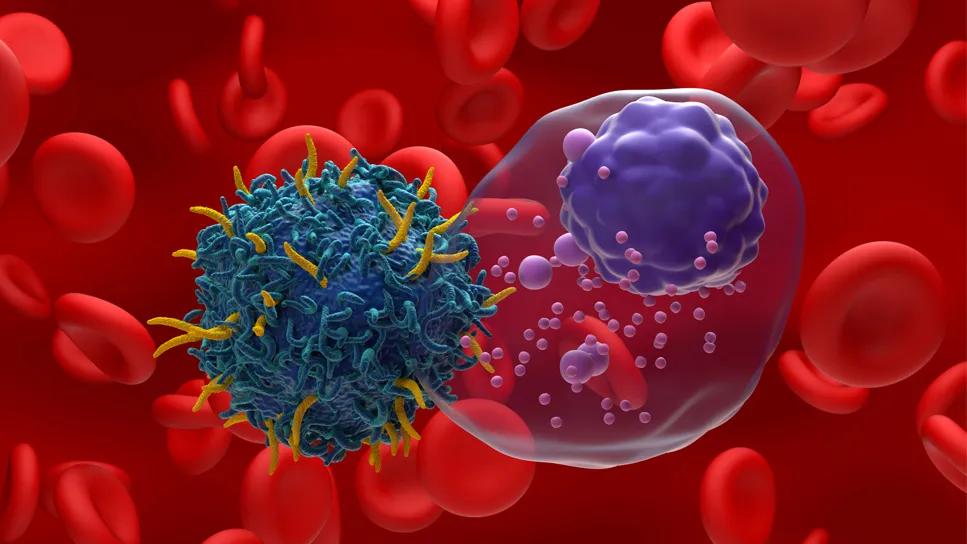
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/b9ed2298-ca45-4a04-acf6-e3c21af05048/rrmm-autologous-car-t-cell-therapy-2176871074)
CAR T-cell therapy
A Cleveland Clinic patient participated in a clinical trial of allogenic CAR T-cell therapy to treat highly resistant multiple myeloma and achieved a complete response. Five years later, her remission has endured. “The duration of response is stunning,” says Multiple Myeloma Program Director Jason Valent, MD.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In the spring of 2018, a 63-year-old retired schoolteacher sought care at Cleveland Clinic after experiencing severe back pain, which was a result of compression fractures throughout her lumbar spine. It turned out that her broken bones were caused by multiple myeloma.
Jason Valent, MD, and Faiz Anwer, MD, led her care team, initially treating her with bortezomib, lenalidomide and dexamethasone, followed by melphalan leading up to a stem cell transplant. She achieved a partial response from the stem cell transplant but relapsed in less than a year. Over the subsequent years, the hematology team tried numerous standard-of-care combination therapies, however, the patient had short-lived remission each time as well as persistent low white blood cell counts.
By late 2020, the team faced a critical junction. “The way the disease was behaving, we knew we needed to come up with something extremely novel,” recalls Dr. Valent. “A clinical trial was opening up at the time to study allogenic CAR T-cell therapy. I discussed the pros and cons with the patient and her husband, who is a retired ER nurse. They both recognized that there were a lot of unknowns since this was a first-in-human study and there were few other treatment options available given that her disease hadn’t responded to the best therapies available.”
One advantage of allogenic CAR T-cell therapy is that there’s no wait time for cells to be manufactured. This helped to accelerate time to treatment. Clinicians also believe that since allogenic (donor supplied) T-cells have not been subjected to years of treatment like autologous T cells have, they may potentially be healthier and more able to fight off myeloma cells.
Advertisement
The patient and her family decided to proceed with the treatment. In November 2020, she was admitted to Cleveland Clinic Cancer Institute. The allogenic CAR T-cells were infused several days later. Like all patients receiving cell therapy, she remained in the hospital for observation to address any emerging side effects. She did not experience cytokine release syndrome (CRS) or immune effector cell-associated neurotoxicity syndrome, both of which are fairly common for these therapies.
The patient did experience severe immunosuppression, resulting in a rare BK viral skin rash over much of her body that caused temporary disfigurement of her face. An inpatient dermatologist was brought in for a bedside consultation. He prescribed an antiviral medication, which brought the rash under control.
“With first-in-human studies you don’t have a full appreciation of the complete toxicity profile of a drug, and that was proven here in terms of the degree of immunosuppression and the viral complications,” says Dr. Valent. “Cell therapies can be really hard on an immune system, with off-target effects that are rather profound.”
The patient also experienced prolonged neutropenia, requiring granulocyte colony-stimulating factor injections on several occasions during her hospitalization. The Palliative & Supportive Care team worked alongside the Hematology team to help alleviate pain and other symptoms. “The palliative doctors are wonderful,” says Dr. Valent. “They are true experts in symptom management, helping people with cancer to live their best lives.”
Advertisement
The patient was discharged home after 12 days. Roughly a month after CAR T-cell therapy, she developed a rash, which was determined to be a side effect of fluconazole. She was readmitted on two occasions for fever. The fevers were not related to CRS but more likely related to her compromised immune system.
After cell therapy, the patient underwent bloodwork and a bone marrow biopsy, which confirmed that she achieved a stringent complete response. In subsequent years, she received bone marrow biopsies to monitor her condition, each confirming the ongoing remission. November 2025 marked five years since her CAR T-cell therapy, and she continues to remain in full remission. “Her response stunned all of us,” says Dr. Valent. She feels fantastic. She loves playing with her grandchildren, and she’s grateful for each day.
In terms of maintenance, she requires monthly IVIG as well as oral antiviral medications to shore up her immune system and protect against shingles and pneumonia. Aside from some residual pain from bone fractures, she has no physical restrictions and has resumed normal daily activities.
“I give so much credit to the cell therapy team for their work on these types of treatments,” says Dr. Valent. “It’s amazing to be part of an institution at the forefront of this work where patients have access to these types of therapies.”
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches