Collaboration critical to a successful resection
In April 2022, a 12-year-old male presented to Cleveland Clinic's emergency department reporting one to two weeks of blurry vision when blowing his nose and one day of complete vision loss in the right eye. He had a bump in his mouth, had been having headaches and nausea for two weeks, and had a long history of nasal congestion and rhinorrhea. At prior visits to urgent care centers, his nasal congestion was diagnosed as allergies.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The exam found a large tumor in his mouth, an afferent pupillary defect in his right eye, a pulsatile mass obstructing the right nasal cavity completely deviating the septum to the left, and an extension of the tumor through the right hard palate.
After inpatient admission, the patient had a T1 MRI (below) that revealed a very large nasal mass abutting the internal carotid arteries and right orbital apex, erosion of the clivus on the floor of the anterior cranial fossa cribiform and involvement of the right pterygoid plates. Unfortunately, given the duration of vision loss in the right eye, return of vision was not possible.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/bb5c810b-df0a-40eb-81c5-350781636567/22-HNI-3505063-PedTumorMultidisciplinaryCase-hero_650x450_jpg)
(Left) Coronal T1 MRI showing a very large nasal mass abutting the internal carotid arteries and right orbital apex. (Center) Sagittal view showing erosion of the clivus, the floor of the anterior cranial fossa cribriform. (Right) Axial T1 showing involvement of the right pterygoid plates.
Because the tumor was so aggressive, a biopsy was performed, which confirmed a diagnosis of juvenile angiofibroma, a benign vascular nasal cavity tumor found exclusively in adolescent males; it often originates from the sphenopalatine foramen. The vascular source is commonly the internal maxillary artery, ascending pharyngeal artery, and/or internal and external carotid arteries. Hormones have been theorized as a possible trigger for tumor growth and angiogenesis; however, the precise mechanism has not yet been elucidated.
“It was the largest and most aggressive angiofibroma I’ve seen reported. We see cases of juvenile angiofibroma, but this was a unique presentation,” says Rachel Georgopoulos, MD, a pediatric otolaryngologist and Director of the Head and Neck Oncology Pediatric Endocrine Center.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/24549612-3166-49ae-a8a8-47dd5faa0e05/22-HNI-3505063-PedTumorMultidisciplinaryCase-inset3_800x537-300x201_jpg)
Endoscopic view showing extension of mass to bilateral nasal cavities, sinuses, nasopharynx, right pterygopalatine fossa, cribriform and planum.
To prepare for surgical resection, embolization of the bilateral internal maxillary arteries was performed by interventional neurology. Due to the tumor’s large size and penetration into surrounding tissue that is seen more often in adults, the surgical team included two surgeons from the adult service: neurosurgeon Varun Kshettry, MD, and rhinologist and skull base surgeon Raj Sindwani, MD, who have deep experience operating on tumors at the skull base. In case a flap was needed to repair a fistula in the oral cavity, adult head and neck surgeon Brandon Prendes, MD, was ready to assist.
Advertisement
“Juvenile angiofibroma isn’t usually life-threatening, but this case could have been since the tumor abutted major vessels, nerves and arteries. At Cleveland Clinic, we can provide resources that might not be possible at a medical center that doesn’t have both pediatric and adult services that handle such complex cases,” says Dr. Georgopoulos.
Together, the surgical team performed an endonasal resection that included an early septectomy to allow for bimanual access through the nose, extensive tumor debulking with a coblator, and clipping of the bilateral sphenopalatine arteries.
The tumor was dissected from the nasal floor and palate (see below), leaving the palate intact; also dissected were the right pterygoids.
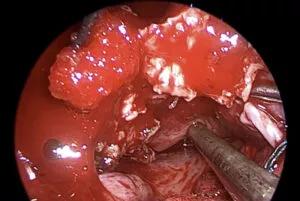
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/f7c64033-6455-4579-b072-056b0aae9167/22-HNI-3505063-PedTumorMultidisciplinaryCase-inset1_800x537-300x201_jpg)
Endoscopic view showing dissection off of the nasal floor and palate. The known expansile site of hard palate is identified.
The team used a high-speed drill to take down the medial pterygoid plate and performed a coblation of the mass medial to the lateral pterygoid plate, which allowed the tumor to be delivered through the patient’s mouth. Also needed was a planum reconstruction with a free mucosal graft. Fortunately, the dura was intact (see below). Due to the extensive bleeding during surgery, the patient required seven units of blood.
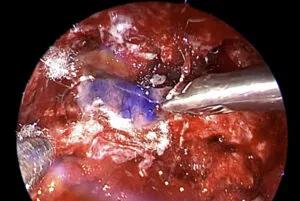
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0306c83c-3f14-4dd9-a631-073772a1687b/22-HNI-3505063-PedTumorMultidisciplinaryCase-inset2_800x537-300x201_jpg)
Endoscopic view showing planum reconstruction with free mucosal graft. The dura remained intact.
The patient was discharged on postoperative day 4, and his headaches and nasal congestion resolved.
Postoperatively he had a small residual tumor. There was again growth that required repeat embolization and a second procedure performed by the same surgical team. He was discharged after three days with very minimal symptoms. His most recent MRI showed gross total resection with minimal enhancement of the right carotid canal, which will be closely monitored.
Advertisement
“What makes this case remarkable is the successful, seamless collaboration across multiple institutes in both the pediatric and adult service lines,” says Dr. Georgopoulos.
Advertisement
Advertisement

Challenging case requires outside-the-box approach

Prompt, multidisciplinary care helps navigate the complexities of a rare condition

Study provides Class III evidence that assay distinguishes disease from normal controls

The tumor's proximity to critical structures made the case challenging

New research adds to understanding of an understudied link

The disorder can greatly impact patients’ quality of life, but sclerotherapy and a multidisciplinary approach to care can be life-changing

The Head & Neck Institute will make its initial footprint in the newly constructed BioRepository building

Randomized controlled trial finds no quality-of-life benefit after standard pituitary tumor surgery