Safety and efficacy demonstrated in largest case series reported to date
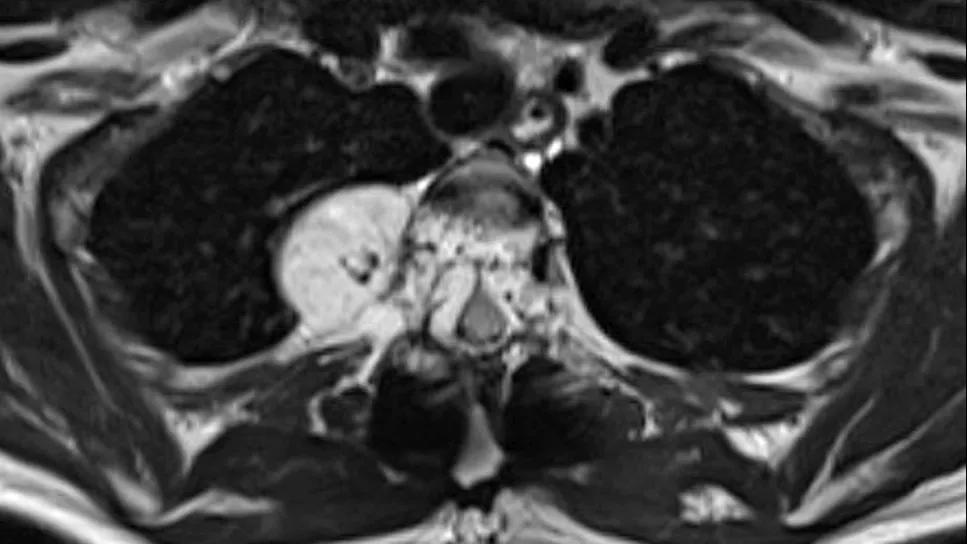
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/eeba0a7a-e0f7-4c4d-91e5-d2fa98e43c48/spinal-hemangioma-on-mri-hero)
vertebral hemangioma on MRI
Spine stereotactic radiosurgery (sSRS) appears to be a safe and effective noninvasive treatment for patients with symptomatic vertebral hemangiomas with epidural extension (SVHEE), whether used as monotherapy or after surgical decompression. So concludes a retrospective review of patients with the rare condition published by Cleveland Clinic researchers in Neurosurgery (Epub 2024 Apr 19).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“This represents what we believe is the largest reported single-center series of patients treated with spine stereotactic radiosurgery for symptomatic vertebral hemangiomas with epidural extension,” says Lilyana Angelov, MD, Head of the Section of Spinal Tumors at Cleveland Clinic, who served as the series’ senior and corresponding author. First author was Arpan Patel, MD, a chief neurosurgery resident at Cleveland Clinic.
“While prospective studies in larger patient samples are still needed to better define the role of sSRS in these patients,” Dr. Angelov notes, “these data are an encouraging addition to the limited existing evidence in support of this more effective alternative to external beam radiotherapy, which is also safer than a number of more invasive procedures, including spine surgery. This appears to be a game-changing therapy in appropriately selected patients whose vertebral hemangiomas cause symptoms due to extension into the epidural space and the adjacent spinal cord.”
Although spinal hemangiomas are the most frequently encountered benign primary tumors of the spinal column, symptomatic hemangiomas with extension into the epidural space are rare. “These symptomatic cases where the mass extends beyond the protective bone and compresses the spinal cord, causing neurological issues, are very infrequent,” Dr. Angelov notes.
She adds that while management of most spinal hemangiomas is more straightforward, treatment of these symptomatic cases can be challenging and often requires a multimodal approach that includes surgical decompression combined with one or more of the following: endovascular embolization, percutaneous vertebroplasty or radiotherapy.
Advertisement
External beam radiotherapy (EBRT) has traditionally been the radiotherapy used for cases of SVHEE. While EBRT has demonstrated good efficacy against symptoms in this setting, it requires administration over multiple days and its use has been linked to heightened risk of secondary cancers over long-term follow-up. This raises concern over potential malignant transformation of this benign pathology as well as potential development of new cancer.
Such concern has prompted interest in the use of sSRS for SVHEE, as sSRS has seldom been associated with neoplasm development and offers a favorable side effect profile relative to EBRT, owing to the highly targeted localized radiation delivery achieved with sSRS.
Since the first reported use of sSRS for SVHEE in 2009, some centers — including Cleveland Clinic — have considered sSRS in lieu of EBRT in the management of SVHEE. “In contrast to EBRT, sSRS is delivered in a single day as a precise, high-dose focal treatment, which can result in better delivery of biologically effective doses to the target region,” Dr. Angelov explains. “This minimizes complications and the risk of delivery of radiation to nearby normal radiation-sensitive structures.”
Despite these suspected benefits of sSRS in this setting, literature on its use has been limited to small case series.
The current series comprised all patients with SVHEE who were treated with sSRS at Cleveland Clinic from 2007 to 2022. The researchers analyzed patient demographics, clinical presentation, lesion volume and spinal cord compression — the latter to directly assess the epidural component of the lesion. Patients’ clinical and radiographic responses and treatment outcomes were assessed at first follow-up (at approximately six months) and at final follow-up.
Advertisement
Over the study period, 14 patients with SVHEE received sSRS as part of their treatment. All received 16 to 18 Gy as single-fraction (one-time) treatment. Nine patients underwent surgical decompression before sSRS, while five patients were treated with sSRS alone.
All patients showed a clear response, with sSRS treatment demonstrating MRI improvement (n = 10) or stability (n = 4) in the spinal compression score from baseline to last follow-up.
Specifically, over mean follow-up of 24 months, median lesion volumes were as follows:
Among the nine patients who underwent surgical decompression and sSRS, eight experienced improvement in myelopathic, radicular and/or pain symptoms and one patient reported stable radiculopathy. Among the five patients who received sSRS monotherapy, two had stable radicular pain and three had improvement in myelopathic symptoms and pain.
In total, 11 of the 14 patients reported symptom improvement following treatment. The three patients who did not report symptom improvement had lesions distal to the conus medullaris (at L3, L5 and S1).
No patients reported major adverse events or long-term symptom worsening after treatment. The figure below presents longitudinal imaging findings from one patient in the series.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/213c4f45-9cc0-4220-82e8-b667e56ab898/spinal-hemangioma-on-mri-inset)
MRI findings from a patient found to have a T3 hemangioma with epidural compression who underwent initial T2-4 decompression and fusion. (A) Initial imaging after surgical decompression, before sSRS treatment. (B) Imaging at one year after sSRS showing reduction in epidural compression and lesion volume. (C) Imaging at two years after sSRS showing further reduction in epidural compression and lesion volume.
“We found that sSRS yielded significant reductions in hemangioma volume in all patients as well as significant reductions in epidural compression and neurological symptoms and pain in a large majority of patients,” Dr. Angelov notes. “Given the unprecedented size of our reported case series, this is one of the strongest data sets to date in support of safety and efficacy of sSRS for symptomatic hemangiomas extending into the epidural space.”
Advertisement
Dr. Angelov emphasizes several notable aspects of her group’s findings:
While the researchers are buoyed by these results, Dr. Angelov acknowledges that this report is limited by its still relatively small size, retrospective nature and two-year follow-up. “Larger prospective studies would be helpful to further assess the role and safety of sSRS in this setting, and longer follow-up is needed,” she concludes. “The latter point is particularly pertinent in view of the benign nature of these hemangiomas, where the continued efficacy of the treatment and any unexpected long-term toxicity must be carefully evaluated.”
Advertisement
Advertisement
Insights from 15 years of experience of Cleveland Clinic’s spine tumor board
Success for these complex operations requires judicious patient selection and presurgical patient optimization
Meta-analyses signal an opportunity to reshape risk stratification and surgical protocols for these comorbidities
A host of factors shape when to intervene and which of three primary procedures to use
Tool correlates well with sagittal vertical axis and quality-of-life measures
Two-year trial results find Total Posterior Spine System to be safe and effective
Minimally invasive approach is gaining prominence as a fast and safe outpatient procedure
Insights on leveraging collaboration and advocacy to develop and conduct needed trials