Combining quantitative vessel wall MRI metrics, CSF abnormalities and neurologic symptoms can be highly predictive
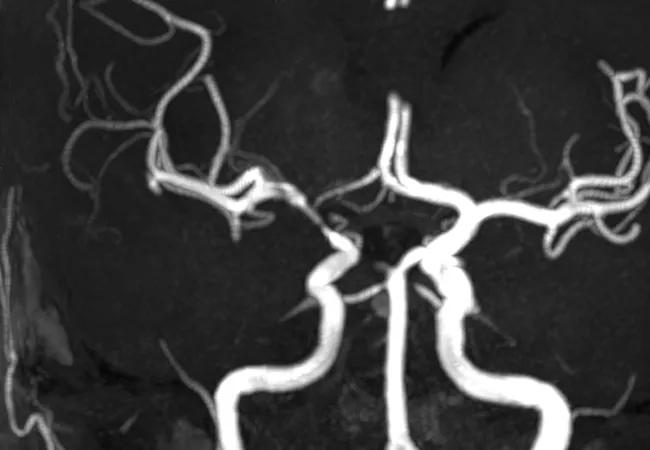
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c66b8908-9c2e-49fa-a1a4-62d9c2214c04/17-RHE-1241-Hajj-Ali-Hero-Image-650x450pxl_jpg)
brain vessels in primary angiitis of the CNS
An observational study has identified several predictors for effectively differentiating primary angiitis of the central nervous system (PACNS) from intracranial atherosclerotic disease (ICAD) as a causative factor in patients who have suffered ischemic stroke due to vasculopathy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The study, published by Cleveland Clinic investigators in the August issue of Neurology: Clinical Practice, found that quantitative vessel wall magnetic resonance imaging (VWMRI) metrics, cerebrospinal fluid (CSF) pleocytosis and clinical features of encephalopathy, seizure and headache all significantly predicted a diagnosis ofPACNS over ICAD.
“For the first time and in the largest study of vasculopathy patients with vessel wall imaging to date, we have used quantitative metrics rather than qualitative interpretation of VWMRI, alongside CSF and other clinical variables, to predict PACNS and differentiate it from ICAD,” says first author G. Abbas Kharal, MD, MPH, a vascular neurologist and neuroimmunologist in Cleveland Clinic’s Cerebrovascular Center. “Our results show that the combination of all these factors can be used to reliably identify PACNS.”
Identifying PACNS in stroke patients with vasculopathy is challenging because no imaging features or clinical hallmarks have previously distinguished it from ICAD in a reliable manner. Diagnostic criteria for PACNS have focused on visualization of arterial irregularities on vessel contour imaging; however, these scans provide little information about vessel wall changes or intrinsic arterial wall pathology.
Tissue sampling remains the gold standard for diagnosis, but it has low sensitivity for PACNS (53% to 74%), given sampling error. Biopsy also is invasive, and the area of most interest may be too deep to reach safely, or results may be inconclusive. As a result, clinicians frequently resort to a combination of clinical, CSF and imaging markers to distinguish PACNS from ICAD.
Advertisement
VWMRI has been increasingly studied for differentiating inflammatory from noninflammatory vasculopathies. To date, however, no quantifiable predictors of PACNS on VWMRI have been identified. Research also is lacking about which combinations of clinical, CSF and VWMRI markers might be most effective for diagnosis when brain biopsy is unobtainable or inconclusive.
To fill that evidence gap, Dr. Kharal and colleagues conducted a cross-sectional study of adults evaluated between January 2015 and December 2021 for inflammatory intracranial vasculopathy as a possible underlying cause of stroke. All patients had evidence of ischemic stroke on brain CT or MRI and of intracranial vasculopathy on vessel contour imaging.
An ICAD or PACNS diagnosis was required. Presence of vascular risk factors, VWMRI findings suggestive of atherosclerotic plaque, available CSF studies showing normal cell counts, and 12 months of clinical and radiographic follow-up data were the basis for ICAD diagnosis. PACNS diagnosis was based on biopsy or expert adjudication of evidence from clinical data, imaging, CSF studies and systemic workup to exclude secondary causes of vasculitis.
Variables analyzed were patient demographics, vascular risk factors, presenting symptoms, serologic parameters, findings from CSF studies and VWMRI, infarct patterns on MRI and any available brain biopsy results.
Thirty-two patients with ICAD and 27 with PACNS were included, six of whom had undergone biopsy. Twenty-four of the patients with ICAD, and six with biopsy-proven PACNS, had large-vessel involvement and made up the cohort for the primary analysis.
Advertisement
A significant association was found between PACNS and encephalopathy as well as seizure. Sensitivity analysis of all patients revealed that headache was a significant predictor of PACNS.
“Encephalopathy and seizures were associated with PACNS in the unadjusted primary analysis, but not in biopsy-proven cases with large vessel involvement when adjusted for age, sex and race,” says Dr. Kharal. “Presence of headaches, however, did significantly differentiate PACNS in the sensitivity analysis, regardless of vessel involvement.”
The likelihood of PACNS increased by 47% for every 1 white blood cell/µL increase in CSF, a finding that held irrespective of vessel type or biopsy. No specific or statistically significant association was seen between CSF protein and PACNS. “CSF protein elevation can be nonspecific, which is likely why it wasn’t a differentiating variable associated with PACNS in our study,” Dr. Kharal observes.
VWMRI findings shown to be predictors of significantly higher odds of PACNS versus ICAD were as follows:
“Predominance of vessel irregularity is a hallmark of ICAD,” Dr. Kharal notes, “whereas higher concentricity and less irregularity are strongly predictive of PACNS.”
The study is limited by its cross-sectional design, small sample size, highly selective patient population and reliance on available data from medical chart review. The VWMRI metrics may only be applicable to patients with large vessel involvement. Nevertheless, the authors say, the results have immediate application for clinicians who encounter stroke patients with cerebral vascularity, suspect PACNS and need to distinguish it from ICAD.
Advertisement
“When tissue diagnosis with brain biopsy is too high-risk or results from it are inconclusive, the combination of factors we’ve described can provide valuable information,” Dr. Kharal says. “Moreover, our results call for revision of previous diagnostic criteria for probable PACNS, which rely mainly on clinical features and angiographic abnormalities on invasive cerebral angiogram after ruling out secondary causes.”
He concludes: “In the real world, improved diagnostic accuracy with these factors may help minimize misdiagnoses and prevent unnecessary invasive testing or immunosuppression initiation in individuals with noninflammatory vasculopathy.”
Advertisement
Advertisement
OCEANIC-STROKE results represent long-sought advance in secondary stroke prevention
Distinct MRI signature includes lesions beyond the corpus callosum, features predictive of vision and hearing loss
Aim is for use with clinician oversight to make screening safer and more efficient
Tasked-based therapy improves social connection and quality of life
LAA closure may be compelling option in atrial fibrillation ablation patients at high risk of both stroke and bleeding
Case illustrates essentials of the low-risk, high-potential procedure when paired with rehab
New analyses confirm preservation of ablation outcomes, broaden data on bleeding benefits
Increasing treatment options are extending the window for continued functional gains