Collaboration is key to expanding access for patients

Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Facial deformities and paralysis due to trauma, tumors or developmental etiologies are commonplace throughout the world. These disorders incur massive social and psychological costs and prevent children and adults from living healthy, confident lives.
Furthermore, the lack of access to or knowledge of optimal facial reconstruction after removal of cancers or benign tumors both compromises treatment and discourages individuals from receiving critical and often lifesaving interventions. Access is further complicated by redundant and scattered services (e.g., major reconstruction, scar revision, functional rehabilitation) performed in multiple subspecialty areas within academic medical centers. This lack of coordination and clarity can prevent individuals from understanding and harnessing their full potential to regain a more normal appearance and function.
To address these issues, Cleveland Clinic is forming the Center for Facial Reconstruction and Facial Nerve Disorders, a collaborative undertaking that will serve as a central access point for patients and span more than 15 medical subspecialties. The center will combine the surgical efforts of Head and Neck Surgery, Facial Plastic and Reconstructive Surgery, Plastic Surgery, Dermatologic Surgery, Neurosurgery, Neurotology, Oromaxillofacial Surgery, and Oculoplastic Surgery. From diagnostic and rehabilitative standpoints, the center also includes neurologists with expertise in facial paralysis and facial pain disorders, neuroradiologists, oromaxillofacial prosthodontists, physical therapists, and speech pathologists. Radiation and medical oncologists play a critical role when cancer concerns remain evident. Here is a full list of collaborators in the Center:
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5cec38ce-8ac6-4c52-bbaf-7439b80b8d71/19-ENT-4286-physicianNamesTable2-800x2010-1_jpg)
By combining energy, expertise and varied perspectives, this unique team-based model will catalyze innovation, yielding new hope of restoring patients to normalcy in areas previously lacking such potential. We envision that this center will lead to novel discoveries and foster new therapies and treatments for patients who experience or are at risk of aesthetic and functional compromise. Our services will range from initial major primary and revision reconstructive surgery to scar revision and restoration of normal function. The main divisions of the center include:
This center aims to harness several unique procedures our team has developed that serve as a platform for further innovation, including those mentioned below.
These innovations have made free tissue transfer a treatment of choice, rather than an avoided “last resort” operation, in many instances. By minimizing the physical and financial costs of this highly technical auto transplantation technique, we are expanding indications to less life-threatening deformities such as palate fistulas and facial contour defects, thus allowing patients to rapidly and reliably return to a more normal function and appearance.
Advertisement
No routine and effective procedure has existed to stop the devastating long-term effects of advanced ORN, which fails hyperbaric oxygen treatment before it progresses and requires extensive reconstruction. This technique provides new and robust circulation to damaged tissue and halts the destructive process, using low-morbidity fascia lata flaps and minimal access techniques.
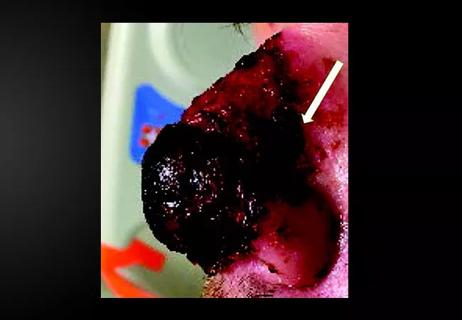
Complete replacement of a missing nose (from cancer or trauma) represents one of the most daunting challenges in facial reconstruction. New techniques that utilize free fascia flaps to provide a thin vascular lining allow for more rapid and optimal restoration of appearance and breathing.
This innovative method has made possible near-total replacement of the orbit, midface and palate, preserving normal appearance and allowing for implant-based dental restoration.
Using this combined technique, we are able to restore facial contour, support and nerve function in the setting of advanced parotid cancers. Patients are spared devastating long-term deformity and dysfunction.
Ultimately, these efforts will enable patients to enjoy the independence and quality of life that normal facial form and function afford. The Center for Facial Reconstruction and Facial Nerve Disorders will continue to seek to advance surgical techniques, expand patient access using telemedicine, and develop cutting-edge research and educational programs. The center will also include a charitable program to provide reconstructive services to patients who are in financial need.
Advertisement
Dr. Fritz is Section Head, Facial Plastic and Microvascular Surgery in Cleveland Clinic’s Head & Neck Institute
Advertisement
Advertisement

Family history may eclipse sun exposure in some cases

Consider secondary syphilis in the differential of annular lesions

Persistent rectal pain leads to diffuse pustules

Two cases — both tremendously different in their level of complexity — illustrate the core principles of nasal reconstruction
Stress and immunosuppression can trigger reactivation of latent virus

Low-dose, monitored prescription therapy demonstrates success

Antioxidants, barrier-enhancing agents can improve thinning hair