Minimally invasive procedure allows surgeons to remove orbital and intracranial tumors without the need for a craniotomy
A minimally invasive procedure that allows surgeons to access and remove certain intracranial tumors near the front of the skull without the need for craniotomy has been performed at Cleveland Clinic for the first time. The procedure, called transorbital neuroendoscopic surgery (TONES), was the result of collaboration between surgeons from Cleveland Clinic’s Head & Neck Institute and the Neurological Institute.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 62-year-old woman who had previously undergone a craniotomy for resection of a meningioma at an outside institution presented to the Cleveland Clinic with bulging of her eye. At her previous surgery, the meningioma had not been fully removed and had since begun to increase in size. When she presented, her left eye was being pushed out (proptosis) due to an intraosseous meningioma in the sphenoid bone. Her symptoms prompted Pablo Recinos, MD, a neurosurgeon in Cleveland Clinic’s Neurological Institute, to order a CT scan and MRI, which confirmed the location of the meningioma that was causing the proptosis. Given the location of the tumor, she was a candidate for the TONES procedure, which was scheduled soon after the initial visit with the patient. Dane Genther, MD, a facial plastic and microvascular surgeon in the Cleveland Clinic’s Head and Neck Institute, performed the approach for the surgery and provided exposure of the tumor for Dr. Recinos.
Video content: This video is available to watch online.
View video online (//www.youtube.com/embed/P4XoKXUio-M)

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a180cc19-4b98-49c0-b2b9-2189f125f0d8/21-HNI-2078116-TONES-Genther-Recinos-surg2-CQD-_650x450-300x208_jpg)
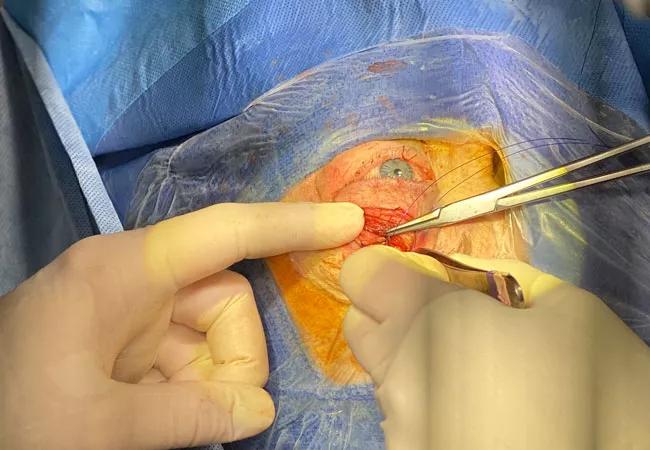
Closing the incision
For the approach, an incision was made in a natural crease in the patient’s upper eyelid. This incision placement is chosen so that it is mostly hidden postoperatively. From there, Dr. Genther went through the skin and muscle to get down to the orbital septum and periosteum. Periosteum was then incised at the level of the orbital rim, and orbital contents were elevated in an atraumatic fashion until the tumor was adequately exposed. At this point, Dr. Recinos took over and removed the tumor. This included soft tissue around the eye as well as bone that had been thickened by the tumor and that was putting pressure on the eye causing it to be pushed out. Once the tumor was removed, the eyelid was carefully reconstructed and the incision closed.
Advertisement
TONES is a relatively new technique, but it is becoming a first-line treatment option as more surgeons become trained to perform it. It is ideal for patients with tumors of the orbit, frontal sinus, anterior cranial fossa, sphenoid bone and anterior-lateral parts of the middle cranial fossa.
“TONES is meant to access certain tumors in different parts of the skull or brain through the eyelid or around the eye that, in the past, would have required a bigger surgery with a craniotomy and removal of part of the bone for access,” says Dr. Recinos. “This is a minimally invasive approach to access certain brain tumors near the front of the skull.”
Video content: This video is available to watch online.
View video online (//www.youtube.com/embed/vCw28i-i6yc)
In the past, patients with intracranial tumors required invasive surgery and an extensive recovery period, both of which increase the chance of post-operative complications. “Conventional surgery requires a fairly large incision in the scalp because you need to remove part of the cranial bone,” explains Dr. Genther. “It can also result in dysfunction and/or wasting of the temporalis muscle. Often in certain locations, you have to retract part of the brain or go through certain structures just for access, which puts those areas at risk. The recovery is also longer because it’s a bigger surgery — the patient stays longer in the hospital, there is more swelling, and there are more risks. By going through the orbit, the surgeon may actually have to violate fewer structures to get to the tumor.”
Beyond the risk reduction during surgery and recovery, there are additional benefits for the patient. Because TONES is much less intrusive than the conventional approach, there is less of a cosmetic impact on the patient. “Although most tumors can be removed with the conventional approach, the recovery is quicker and in this case, specifically, her incision was just in her eyelid,” says Dr. Genther. “Once she healed after surgery, the incision was barely visible. Plus, since we didn’t have to go through important adjacent structures, we didn’t need to take off bone and put bone back on, which is what the neurosurgical team would otherwise have to do.”
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/9992df46-51d1-491a-aeea-29480a1a9f7b/21-HNI-2078116-TONES-Genther-Recinos-face-CQD-_650x450-300x208_jpg)
The patient has a barely appreciable incision above her right eye only a few months after her surgery.
Drs. Recinos’ and Genther’s patient only required an overnight stay in the hospital. She had some eyelid swelling, but Dr. Genther says that is to be expected. “She didn’t really have any visual problems afterward. Her vision stayed intact, but there was some muscle weakness, which was temporary,” he says. “I saw her about a month after the surgery and she was doing well. Her eyelid was still a little swollen, but the incision had healed nicely. This would have been a different situation if Dr. Recinos and his team had to do redo the craniotomy with a large scalp incision, as would have been the case with the conventional approach.”
Advertisement
Advertisement

Aim is for use with clinician oversight to make screening safer and more efficient

Rapid innovation is shaping the deep brain stimulation landscape

Study shows short-term behavioral training can yield objective and subjective gains

How we’re efficiently educating patients and care partners about treatment goals, logistics, risks and benefits

An expert’s take on evolving challenges, treatments and responsibilities through early adulthood

Comorbidities and medical complexity underlie far more deaths than SUDEP does

Novel Cleveland Clinic project is fueled by a $1 million NIH grant

Tool helps patients understand when to ask for help