A mortality risk profile based on lymphocyte count, red blood cell distribution width and C-reactive protein levels
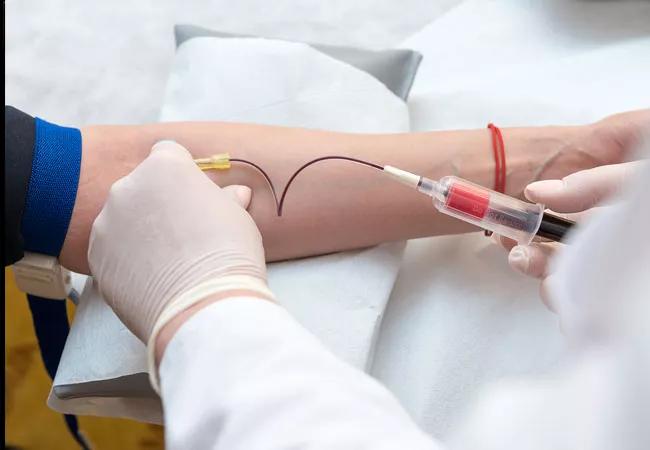
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/553f9019-114a-4025-baa4-1be9be444dda/20-LRI-050-bloodDrawMortalityPredict-650x450_jpg)
20-LRI-050-bloodDrawMortalityPredict-650×450
Commonly used clinical indicators of immune status and inflammation are powerful predictors of mortality in the general population, according to the results of new collaborative, cross-city study led by Cleveland Clinic and University Hospitals.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Published in JAMA Network Open, the team—led by Jarrod Dalton, PhD, an epidemiologist in Lerner Research Institute’s Department of Quantitative Health Sciences, and David Zidar, MD, PhD, an interventional cardiologist and immunologist at University Hospitals Cleveland Medical Center and the Louis Stokes Cleveland Veteran Affairs Medical Center—showed that lymphopenia (a condition characterized by abnormally low levels of a specific type of white blood cell, called lymphocytes) is associated with death due to cardiovascular disease, malignancy and respiratory infections, including influenza and pneumonia. This relationship between lymphocyte levels and mortality was observed independent of age, other blood-based immune markers and clinical risk factors.
“Scientists have gone to great lengths and expense to develop novel biomarkers to identify people at the highest risk for death and disease,” said Dr. Dalton, senior author on the study. “Here we have taken a more pragmatic approach—investigating the prognostic power of components of a patient’s white blood cell count, which is collected as part of routine blood work performed during standard health exams. The complete blood count test is convenient, inexpensive—costing roughly the same as a couple of delivery pizzas—and, as our findings suggest, may be used to help physicians screen for and prevent disease and disease-related mortality.”
In this study, the team analyzed data from more than 31,000 participants who were followed over the course of 12 years as part of the National Health and Examination Survey (NHANES). NHANES is a program of the National Center for Health Statistics, part of the Centers for Disease Control and Prevention, and the study participants were representative of the general United States adult population.
Advertisement
While the association between lymphopenia and reduced survival was observed independent of age and traditional clinical risk factors, the strength of the association increased when low lymphocyte levels presented in combination with other blood abnormalities, including elevated red blood cell distribution width (a measure of the body’s ability to generate and maintain a healthy population of red blood cells) and levels of C-reactive protein (an established indicator of inflammation).
Individuals that present with lymphopenia and these other blood abnormalities are needles in a haystack of seemingly healthy adults who are actually at much greater likelihood of developing cancer, heart disease or fatal infections.
Applied in practice, the study’s findings suggest, for example, that a 65-year old with a high-risk profile based on these three immune indicators—lymphocyte count, red blood cell distribution width and C-reactive protein levels—is actually at greater mortality risk than someone who is a decade older and has a low-risk profile.
“With additional research, we will soon begin to understand the biologic processes that link these markers to disease, a critical step in the search for therapeutic targets,” said Sadeer Al-Kindi, MD, a cardiologist at University Hospitals, clinical instructor at Case Western Reserve School of Medicine and co-author on the study. “More immediately, we can certainly design systems that allow physicians to use pragmatic immune status indicators to ensure that the 10-20% of the general population at highest risk for mortality do not fall through the cracks of routine preventive care and early detection services.”
Advertisement
This study was a collaboration between members of the Clinical and Translational Science Collaborative (CTSC) of Cleveland, including researchers from Cleveland Clinic, University Hospitals, Case Western Reserve University, Louis Stokes Cleveland Veterans Affairs Medical Center and MetroHealth Medical Center. The CTSC Awards Program is administered through the National Center for Advancing Translational Sciences, part of the National Institutes of Health (NIH). This study was also supported by the National Institute of Aging, of the NIH.
Advertisement
Advertisement
First full characterization of kidney microbiome unlocks potential to prevent kidney stones
Researchers identify potential path to retaining chemo sensitivity
Large-scale joint study links elevated TMAO blood levels and chronic kidney disease risk over time
Investigators are developing a deep learning model to predict health outcomes in ICUs.
Preclinical work promises large-scale data with minimal bias to inform development of clinical tests
Cleveland Clinic researchers pursue answers on basic science and clinical fronts
Study suggests sex-specific pathways show potential for sex-specific therapeutic approaches
Cleveland Clinic launches Quantum Innovation Catalyzer Program to help start-up companies access advanced research technology