A model for critical evaluations of surgical procedures

By Edmund Sabanegh Jr., MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
With continued growth in healthcare costs, there is a strong push for providers to look critically at per-case costs to identify opportunities for efficiencies. This is particularly important in the arena of elective procedures, where patients may bear a significant financial burden in the form of high deductible insurance plans, copayments and noncoverage.
One of our areas of focus in Cleveland Clinic’s Department of Urology has been to critically analyze our procedural costs, with an eye toward reducing variable costs without compromising the efficacy of the procedure. Our most recent efforts have involved a careful comparative analysis of our costs for reproductive microsurgery.
Vasectomy remains a major contraceptive technique throughout the world, with more than 500,000 vasectomies performed in the United States each year. For couples who desire conception after vasectomy, vasectomy reversal with microsurgical vasovasostomy remains the gold standard in terms of outcomes and safety, with as many as 6 percent of vasectomized men choosing to pursue this approach.
For most patients, these surgeries are expensive and usually not covered by insurance plans. Costs are primarily driven by lengthy microsurgical procedure times and expensive specialized sutures.
Multiple variations in reconstructive approach have been described for vasovasostomy, but the formal two-layer microsurgical technique remains the gold standard, producing excellent outcomes with respect to patency and pregnancy rates.
Advertisement
Large multicenter trials have shown equal efficacy for a simpler, modified one-layer approach. Because of the greater microsurgical precision, the formal two-layer anastomosis tends to have longer operative times, with requirements for more microsurgical suture (10-0 vs. 9-0) than the modified one-layer repair.
We conducted a comparative cost analysis of 106 patients on whom one of the two different techniques were performed between 2010 and 2015. The two groups were statistically similar in age and time since vasectomy. Specific attention was given to operative times, suture requirements and postoperative outcomes (semen parameters). Cost and surgical outcomes are summarized in Figure 1.
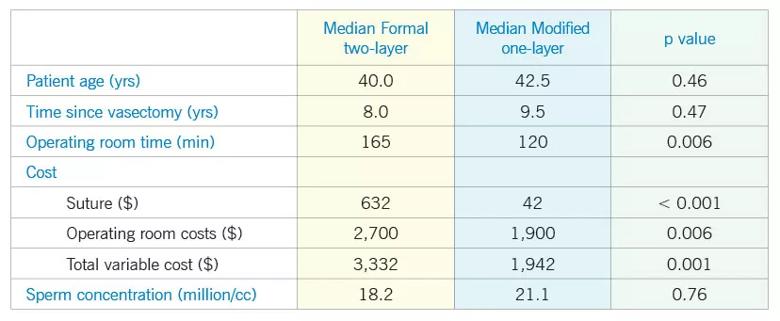
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/c0ac0ab1-c988-45e5-ad65-b28482c7579d/Inset-Chart-Medical-Cost_jpg)
Figure 1. Comparative cost and surgical outcomes for vasovasostomy techniques.
Modified one-layer microsurgical reconstruction resulted in shorter operative times and lower disposable and overall cost when compared with formal two-layer vasovasostomy. These efficiencies were accomplished without compromising the efficacy of the procedure as defined by semen parameters.
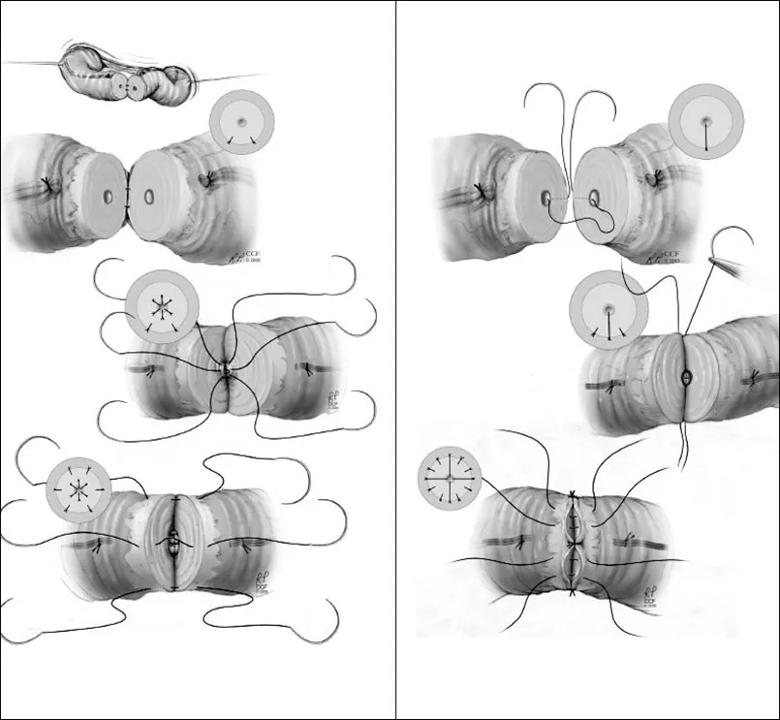
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a992f814-4c8d-4b38-ad83-1a2c87124f06/Sabaneh-Inset_jpg)
Figure 2: Formal two-layer vasovasostomy Figure 3: Modified one-layer vasovasostomy.
Ultimately, our challenge across the medical profession remains to deliver the highest-quality affordable care. Our comparative cost analysis of vasectomy reversal is just one step in our journey to make procedures more available to patients who are shouldering an increasing economic burden in healthcare.
Safarinejad M, Lashkari M, Asgari S, Farshi A, Babaei A. Comparison of macroscopic one-layer over number 1 nylon suture vasovasostomy with the standard two-layer microsurgical procedure. Human Fertil. 2013;16(3):194-199.
Advertisement
Sharma V, Le BV, Sheth KR, et al. Vasectomy demographics and postvasectomy desire for future children: results from a contemporary national survey. Fertil Steril. 2013; 99(7):1880-1885.
Nyame Y, Babbar P, Almassi N, Polackwich A, Sabanegh Jr E. Comparative Cost-Effectiveness Analysis of Modified 1-Layer versus Formal 2-Layer Vasovasostomy Technique. J. Urol. 2015 Sep 24. pii: S0022-5347(15)04802-8. [Epub ahead of print]
Reprinted with permission from Elsevier from Nyame YA, Babbar P, Almassi N, Polackwich AS, Sabanegh E. Comparative Cost-Effectiveness Analysis Modified 1-Layer versus Formal 2-Layer Vasovasostomy Technique. Urol. 2015 Sep 24. Pii: S0022-5347(15)04802-4808. [Epub ahead of print.]
Advertisement
Advertisement

Pediatric urologists lead quality improvement initiative, author systemwide guideline

Fixed-dose single-pill combinations and future therapies

Reproductive urologists publish a contemporary review to guide practice

Two recent cases show favorable pain and cosmesis outcomes

Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood

Proteinuria reduction remains the most important treatment target.

IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy

Oncologic and functional outcomes are promising, but selection is key