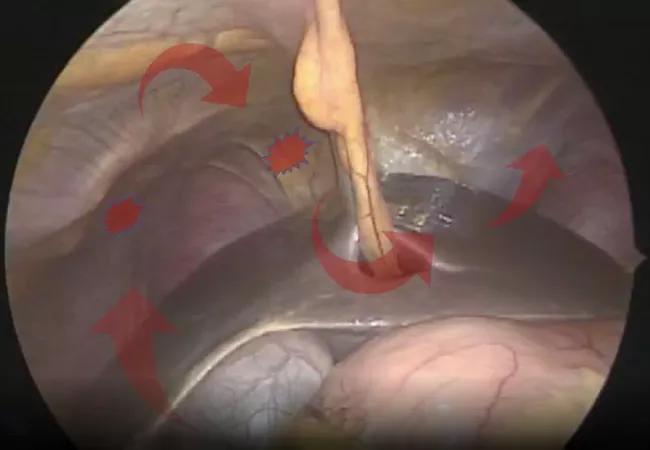
Tips and techniques to help optimize resection and ablation of lesions in the diaphragm
Endometriosis is a common condition, affecting approximately 11% of American women of reproductive age, according to the U.S. Department of Health and Human Services’ Office on Women’s Health. Occasionally, endometrial-like glands and stroma can be found outside the uterine cavity in the pleura, lung and diaphragm.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Diaphragmatic endometriosis is the most common type of extra pelvic endometriosis,” says Miguel Luna, MD, a Cleveland Clinic physician. “However, it is very rare – about 12% of women with pelvic endometriosis may present with concomitant diaphragmatic endometriosis – and not a lot of surgeons have exposure to the condition.”
As an endometriosis specialist, Dr. Luna sees a higher volume of complex cases. He shared insight into surgical management of diaphragmatic endometriosis in a video article in the Journal of Minimally Invasive Gynecology (JMIG), which won the 2021 JMIG Best Video Award.
A large percentage of patients with diaphragmatic endometriosis are asymptomatic. Those who are symptomatic may experience cyclic shoulder pain, right upper quadrant pain, catamenial pneumothorax and hemoptysis or pleural effusion.
“Diaphragmatic endometriosis can be managed medically,” says Dr. Luna. “Surgery is generally reserved for patients who have significant symptoms or for whom medical management has failed.”
Ablation or resection of diaphragmatic endometrial lesions is typically done via laparoscopy. Surgeons performing the procedures must be familiar with diaphragmatic, liver and thoracic anatomy. Before surgery, patients should undergo diagnostic imaging, preferably magnetic resonance imaging, to map suspicious lesions.
“If the lesion is isolated to the diaphragm alone and you are confident the pleura and lung are not affected from the pre-operative workup, then video assisted thoracoscopic surgery (VATS) is not generally indicated,” says Dr. Luna.
Advertisement
VATS is often performed at the same time as pelvic procedures for endometriosis.
“We usually have a thoracic surgeon on the team working with us,” says Dr. Luna. “Once the abdominal and pelvic portions of the surgery are complete, then the thoracic surgery team takes over. We reposition the patient, and the thoracic team proceeds.” The surgeon then makes a small incision between the rib spaces to insert the video camera and perform the ablation or resection of thoracic lesions, if present.
Dr. Luna offers advice for surgeons who are considering adding surgical management of diaphragmatic endometriosis to their service:
Advertisement
While surgeons at Cleveland Clinic routinely perform concomitant thoracoscopy when diaphragmatic endometriosis is addressed, Dr. Luna urges surgeons to schedule separate pelvic and diaphragmatic endometriosis excisions if the right team isn’t in place. “Don’t feel compelled to do both at the same time,” he says.
Finally, Dr. Luna encourages gynecologists and gynecological surgeons to listen to their patients.
“We see a lot of patients who present with symptoms of diaphragmatic endometriosis that have been in pain for a very long time,” he says. “Diaphragmatic endometriosis may be uncommon, but it can be debilitating. It’s important to have a high index of suspicion when symptoms are present, conduct a complete medical examination and refer the patient for management when appropriate.”
Advertisement
Advertisement

Uterine transposition cleared the field for radiation therapy

ACOG-informed guidance considers mothers and babies

Prolapse surgery need not automatically mean hysterectomy

Artesunate ointment shows promise as a non-surgical alternative

New guidelines update recommendations

Two blood tests improve risk in assessment after ovarian ultrasound

Recent research underscores association between BV and sexual activity

Psychological care can be a crucial component of medical treatment